Virtual AI Urgent Care Assistant: Rapid Triage and Smart Diagnostics for Telehealth
Telehealth’s rapid growth has transformed urgent care, but a persistent challenge remains: clinicians spend significant time gathering and interpreting disparate patient histories before they can provide meaningful care. Enter the virtual AI urgent care assistant—a new generation of intelligent tools that pre-summarize patient histories, flag key findings, and suggest differential diagnoses before a telehealth visit even begins. By automating tasks once relegated to manual review and preliminary interviews, these systems are fundamentally improving consult speed, triage accuracy, and the quality of virtual urgent care.

Why Patient History Matters for Urgent Telehealth
In urgent care settings—virtual or in-person—the first step is quickly assembling the patient’s medical history: symptoms, prior conditions, recent treatments, risk factors, and medication use. In telehealth, the challenge is compounded by lack of face-to-face context, incomplete records, and variable patient communication. Missing information can delay care, lead to medical errors, and reduce consult quality.
Modern AI-enabled urgent care platforms use natural language processing (NLP) and machine learning algorithms to draw structured patient histories from EHRs, symptom-checker questionnaires, chatbots, recent lab and imaging results, and previous telehealth notes:
- Automatic summarization: The AI instantly generates concise medical histories, extracting key data such as chief complaint, relevant symptoms, medications, allergies, and comorbidities.
- Contextual alerting: The system highlights critical findings—like recent ER visits, elevated vital signs, or flagged symptoms (e.g., chest pain or shortness of breath).
- Suggested differential diagnoses: By comparing patient data to vast clinical databases, AI recommends possible diagnoses ranked by likelihood, supporting rapid and accurate triage.
- Care pathway recommendations: The virtual assistant can recommend next steps—labs, imaging, or specialist referrals—customized to the patient profile.
How AI Pre-Summarization Works

Clinical Evidence and Real-World Performance
Faster Consults, Better Outcomes
A comprehensive review of AI-integrated telehealth platforms found that automated triage and pre-visit history organization lead to significant time savings and improved patient satisfaction.
- Consult time reduction: The average urgent telehealth visit became 30–45% shorter when pre-summarization tools were used.
- Enhanced triage: AI-enabled platforms direct high-acuity or emergency cases for immediate escalation, reducing inappropriate telehealth encounters.
- Improved accuracy: Providers reported better ability to prioritize care and quickly identify underlying issues thanks to smart diagnostic suggestions.
Cost and Resource Savings
By reducing the time physicians spend gathering histories and making triage decisions, AI assistants:
- Increase provider throughput in urgent care settings.
- Minimize unnecessary in-person ER referrals or repeat telehealth visits.
- Automate documentation for regulatory and billing compliance, reducing administrative work.

Quality Improvements
AI-powered virtual assistant tools demonstrated improved compliance with care quality standards:
- Structured documentation supports follow-up and continuity of care.
- Decision-support improves guideline adherence and reduces diagnostic errors.
- Data from major health systems show a reduction in physician burnout when AI scribed histories and generated initial SOAP notes.
User Experience: For Patients and Providers
Patient Benefits
- Streamlined intake: Patients complete digital questionnaires or interact with secure chatbots before the visit, with intelligent prompts improving detail collection.
- Speed and convenience: Quicker consults, more thorough intake, and personalized care recommendations.
- 24/7 support: AI-driven chat assistants offer real-time symptom checking and care guidance outside provider hours.
Provider Benefits
- Instant access to key data: Physicians enter consults with actionable summaries, including indexed and flagged information.
- Smart documentation tools: AI-generated SOAP notes and progress reports minimize paperwork and after-hours EHR use.
- Differential diagnosis support: Providers receive ranked, adjustable lists of likely conditions, focused questions, and notes on red flag symptoms.
- Efficient triage: Facility-based teams can rapidly stratify patients and direct care appropriately, increasing job satisfaction and outcomes.
Challenges and Solutions
Privacy, Security, and Trust
AI integration raises important concerns:
- Data privacy must be safeguarded through robust encryption, role-based access, and HIPAA/GDPR-compliant systems.
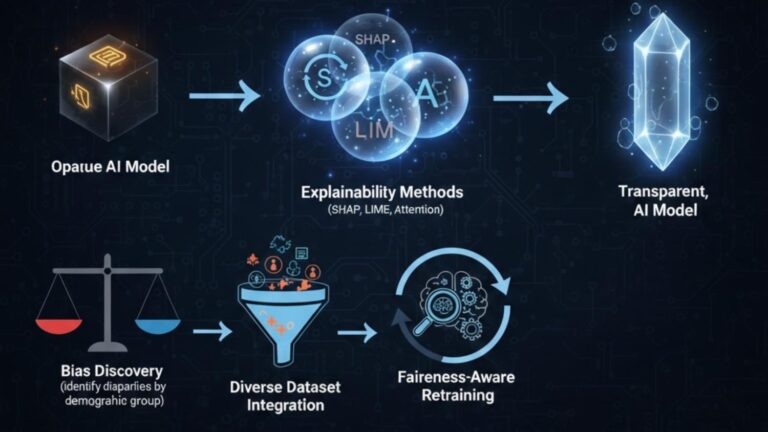
- Explainability is key—platforms must show transparent reasoning for clinical suggestions to foster clinician trust.
Integration with Health Records
To maximize benefit, virtual AI assistants must:
- Integrate with diverse EHRs and telehealth platforms for seamless information flow.
- Maintain interoperability to support complex care transitions (e.g., referrals from urgent care to ER or specialist).
Ethical Considerations
AI should supplement—not replace—clinical decision-making. Systems must:
- Give providers ultimate control and oversight.
- Be transparent about limitations and uncertainty in diagnostic recommendations.

The Future: Smarter, More Adaptive Virtual Care
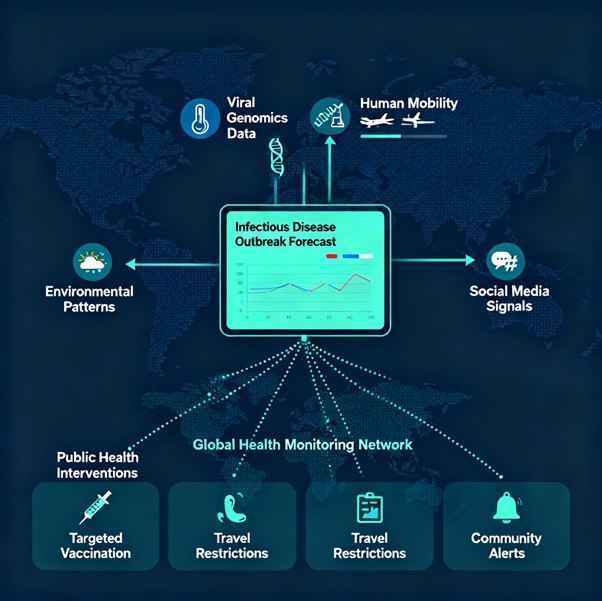
Advancements in generative AI, multimodal reasoning, and ambient listening promise even deeper support:
- Conversational AI can guide both intake and consults, bridging gaps in patient communication.
- Continuous learning allows AI assistants to update triage and diagnostic models using new case data.
- Integration with wearables and remote monitoring devices adds layers of real-time physiologic data to improve early warning and chronic care transitions.