Generative AI in Medical Research: Revolutionizing Rare Disease Trials Through Synthetic Patient Data
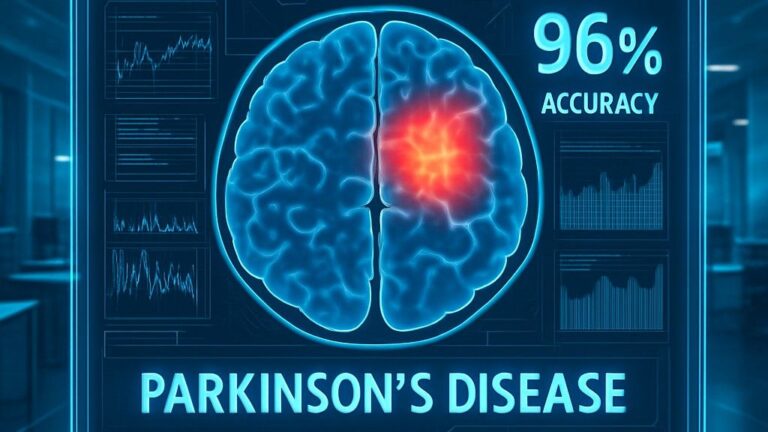
The medical research landscape is experiencing a profound transformation as generative artificial intelligence creates synthetic patient data that promises to accelerate clinical trials, enhance privacy protection, and unlock new possibilities for rare disease research. The SYNTHIA project recently demonstrated that advanced generative AI models can achieve up to 96% data quality scores when creating synthetic medical datasets, while pioneering studies have shown that synthetic cohorts can increase virtual patient populations by threefold while maintaining statistical fidelity to real-world clinical outcomes. This revolutionary approach addresses critical challenges in medical research—from privacy constraints to small patient populations—while opening unprecedented opportunities for personalized medicine and therapeutic innovation.

The Synthetic Data Revolution in Healthcare
Traditional medical research faces fundamental limitations that generative AI is uniquely positioned to solve. Strict privacy regulations like HIPAA and GDPR create significant barriers to data sharing, while rare diseases often affect fewer than 1,000 patients globally, making traditional clinical trials extremely challenging. Generative AI offers a compelling solution by creating synthetic patient data that replicates the statistical properties and clinical patterns of real patient populations without containing any actual patient information.
Foundation Models Transform Healthcare Data Generation
Advanced foundation models specifically designed for healthcare applications are demonstrating remarkable capabilities in synthetic data generation. These systems leverage sophisticated architectures including:
Generative Adversarial Networks (GANs): Creating high-quality synthetic medical images and clinical records with exceptional fidelity to original datasets. Studies show GANs can achieve over 80% accuracy in multi-stage disease classification using synthetic data augmentation.
Variational Autoencoders (VAEs): The Tabular Variational Autoencoder (TVAE) achieved 96% data quality scores when generating synthetic patient heart rate data for privacy-preserving research.
Diffusion Models: Advanced models like DiffWave demonstrate superior performance in generating realistic medical time series data, particularly for cardiac monitoring applications.
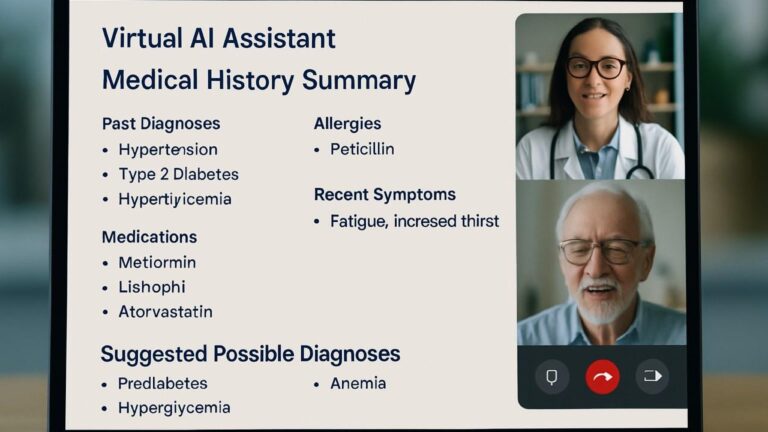
Large Language Models (LLMs): Specialized medical LLMs such as Med-PaLM and BioGPT enable generation of comprehensive clinical scenarios and patient narratives for training and simulation purposes.
Breakthrough Applications in Rare Disease Research
Clinical Trial Acceleration and Enhancement
Synthetic Control Arms Revolution: One of the most impactful applications involves synthetic control arms that replace traditional placebo groups in clinical trials. This approach is particularly transformative for rare diseases where every patient deserves access to potentially life-saving treatments.
Real-World Success Stories:
- Roche’s Alecensa Approval: The EU conditionally approved Roche’s lung cancer treatment using a synthetic control arm of 67 patients, accelerating market access by 18 months
- Pfizer’s Bavencio Trial: The clinical trial for Merkel cell carcinoma treatment used electronic medical records to create synthetic control arms, enabling accelerated FDA approval in 2018
- Amgen’s Blincyto Success: The leukemia treatment received FDA and EMA approval using historical data from 694 patients based on 2,000 patient records for Phase 2 studies
Transformative Impact on Rare Disease Populations
Acute Myeloid Leukemia Breakthrough: A landmark study demonstrated the power of synthetic data in rare disease research by creating synthetic cohorts for acute myeloid leukemia patients that successfully replicated survival curves and complex inter-variable relationships. The synthetic datasets enabled threefold expansion of virtual patient populations while maintaining clinical relevance and statistical integrity.
Myelodysplastic Syndrome Innovation: Researchers used CTAB-GAN+ and normalizing flows (NFlow) to create synthetic cohorts that accurately captured demographic, molecular, and clinical characteristics, significantly enhancing studies on myelodysplastic syndrome. This work reduced research timelines and accelerated clinical advancements by providing robust datasets for analysis.
Alzheimer’s Disease Research: Advanced GANs processing data from 6,919 patients including 64 clinical variables successfully generated synthetic clinical records that forecast disease outcomes with remarkable accuracy. This approach enables comprehensive analysis of neurodegenerative diseases without compromising patient privacy.
Technical Innovations and Performance Achievements
Multi-Modal Synthetic Data Generation
Comprehensive Clinical Simulation: Modern generative AI systems create multi-modal synthetic datasets that combine imaging, clinical data, genomics, and treatment histories. This holistic approach enables:
- Realistic Clinical Scenario Simulation: Including patient demographics, treatment responses, and side effect profiles
- Genomic Data Synthesis: Creating synthetic genomic sequences across different demographics to support precision medicine research
- Longitudinal Patient Trajectories: Modeling disease progression and treatment responses over extended timeframes
Brain Imaging Breakthrough: Researchers developed three-dimensional generative models of human brain imaging that produce diverse, high-resolution, and morphologically preserving samples conditioned on patient characteristics like age and pathology. These models preserve biological and disease phenotypes while enabling use in established image analysis tools.
Privacy-Preserving Methodologies
Digital Twin Architecture: The integration of digital twins with synthetic data generation provides enhanced privacy protection through multiple layers of anonymization. Gaussian Copula (GC) and Tabular Variational Autoencoder (TVAE) models achieved 88% and 96% data quality scores respectively while maintaining complete patient privacy.
Differentially Private Generation: Advanced frameworks employ differentially private GANs that mitigate risks including model inversion attacks and data breaches. These systems enable secure cross-institutional collaboration while maintaining rigorous privacy standards.
Federated Synthetic Data: Privacy-preserving federated learning frameworks allow institutions to collaboratively train generative models without sharing raw patient data, addressing key vulnerabilities including insufficient anonymization and weak access controls.
Regulatory Acceptance and Clinical Validation
FDA and EMA Recognition
Regulatory Support: The FDA has demonstrated increasing acceptance of synthetic data applications, particularly for rare diseases and severe indications without adequate standard of care. Key regulatory developments include:
- Case-by-Case Assessment: FDA guidance emphasizes that synthetic control arm suitability warrants individualized evaluation based on specific clinical contexts
- Evidence Standards: Regulatory bodies require rigorous validation demonstrating that synthetic datasets maintain clinical relevance and statistical properties
- Cross-Border Compliance: Synthetic data facilitates international collaboration by addressing complex GDPR and HIPAA requirements
European Innovation: The Innovative Health Initiative (IHI) funding of the SYNTHIA project demonstrates European commitment to advancing synthetic data methodologies for personalized medicine applications.
Clinical Validation Frameworks
Robust Evaluation Metrics: Successful synthetic data implementation requires comprehensive validation using metrics including mean absolute error, maximum mean discrepancy, and survival curve analysis. Studies consistently demonstrate that high-quality synthetic datasets maintain statistical fidelity while enabling meaningful clinical insights.
Real-World Evidence Integration: Combining synthetic data with real-world evidence enhances research validity and clinical applicability, particularly important for regulatory submissions and clinical decision-making.
Specialized Applications and Innovations
Personalized Medicine Advancement
Precision Therapy Simulation: Generative AI enables personalized therapy simulations that predict individual patient responses to different treatment protocols without requiring extensive clinical trials. This capability is particularly valuable for:
- Rare Genetic Disorders: Where traditional trials are impractical due to small patient populations
- Pediatric Applications: Reducing exposure of children to experimental treatments through virtual modeling
- Complex Comorbidities: Modeling interactions between multiple conditions and treatments
Pharmacovigilance Enhancement: Synthetic data supports comprehensive safety monitoring by generating diverse patient scenarios that capture potential adverse events and drug interactions across different demographic groups.
Advanced Clinical Trial Design
Adaptive Trial Methodologies: AI-generated synthetic datasets enable sophisticated adaptive trial designs that adjust protocols based on interim analyses while maintaining statistical power. This approach is particularly valuable for rare diseases where traditional trial designs prove inadequate.
Endpoint Optimization: The Rare Disease Clinical Outcome Assessment Consortium (RD-COAC) leverages synthetic data to advance measurement tools and methodologies for rare disease clinical trials, addressing the challenge of identifying meaningful endpoints in conditions with limited precedent.
Win Ratio Applications: Advanced statistical methods like win ratio approaches can be enhanced through synthetic data generation that creates diverse patient scenarios for comprehensive treatment effect analysis.
Addressing Implementation Challenges
Quality Assurance and Validation
Fidelity Assessment: Ensuring synthetic data maintains sufficient clinical relevance requires rigorous validation frameworks that assess:
- Statistical Property Preservation: Maintaining correlations and distributions found in original datasets
- Clinical Plausibility: Ensuring generated scenarios reflect realistic medical conditions
- Generalizability: Demonstrating applicability across diverse patient populations and clinical settings
Bias Mitigation: Addressing biases in source datasets is crucial for generating representative synthetic data that supports equitable healthcare research. Advanced frameworks include bias detection and correction mechanisms during the generation process.
Ethical and Regulatory Considerations
Informed Consent Evolution: Synthetic data generation raises important questions about informed consent requirements and patient rights, particularly regarding use of historical data for model training.
Transparency Requirements: Regulatory bodies increasingly emphasize explainable AI methodologies that provide clear insights into synthetic data generation processes and clinical applications.
Global Harmonization: International collaboration is essential for establishing unified standards and ethical frameworks that support responsible synthetic data use across different healthcare systems.
Synthetic Data Clinical Trial Pipeline

Future Implications and Healthcare Transformation
Accelerated Therapeutic Development
Reduced Development Timelines: Synthetic data applications demonstrate potential for dramatically reducing drug development timelines from decades to years by:
- Eliminating recruitment delays through virtual patient populations
- Enabling parallel trial design and optimization
- Supporting regulatory submissions with comprehensive synthetic evidence
Cost Reduction: Substantial cost savings are achievable through reduced patient recruitment requirements, decreased trial infrastructure needs, and accelerated time-to-market for breakthrough therapies.
Global Health Equity
Democratized Research Access: Synthetic data generation enables research institutions worldwide to access high-quality datasets for medical research, regardless of local patient population constraints or privacy regulations.
Underserved Population Research: Synthetic datasets can represent underserved demographics and rare conditions that are typically excluded from traditional clinical trials, promoting more equitable healthcare innovation.
Precision Medicine Evolution
Individual Patient Modeling: The future of medicine lies in creating personalized synthetic patient models that enable individualized treatment optimization and predictive healthcare planning.
Population Health Analytics: Large-scale synthetic datasets support population health modeling and policy analysis while maintaining complete privacy protection and regulatory compliance.
Conclusion: The Synthetic Future of Medical Research
Generative AI’s capability to create high-quality synthetic patient data represents a paradigm shift in medical research methodology. By addressing fundamental challenges including privacy constraints, small patient populations, and ethical concerns, synthetic data generation enables more efficient, ethical, and comprehensive approaches to clinical research.
The convergence of advanced AI architectures, regulatory acceptance, and clinical validation positions synthetic data as a transformative tool for accelerating therapeutic development—particularly for rare diseases where traditional approaches fall short. As healthcare systems worldwide embrace data-driven precision medicine, synthetic data generation will play an increasingly central role in advancing medical knowledge while protecting patient privacy.
The future of medical research is synthetic, and the implications for global health innovation, therapeutic accessibility, and precision medicine are profound. Through responsible implementation and continued technological advancement, generative AI promises to democratize medical research and accelerate the development of life-saving treatments for patients worldwide