The AI Revolution in Clinical Research: From Lab Bench to Bedside, Faster and Smarter

Imagine a world where new life-saving drugs are developed not in years, but in months. A world where clinical trials are more efficient, safer, and tailored to *you*. Sounds futuristic? Perhaps. But consider this: what if the very tools and methods we use to understand and treat disease were themselves becoming intelligent? It’s happening now, thanks to Artificial Intelligence. This isn’t just a technological tremor; it’s a seismic shift that promises to redefine the landscape of clinical research.
1. From Science Fiction to Medical Fact: What is AI in Clinical Research, Anyway?
The concept of Artificial Intelligence often conjures images of sentient robots, but the reality, at least for now, is far more nuanced – and arguably more powerful. At its core, AI is about creating machines that can learn, reason, and solve problems in ways that mimic human intelligence. In the context of clinical research, this translates to harnessing sophisticated algorithms to process and analyze the gargantuan datasets inherent in modern medicine. We’re not just talking about faster calculations; we’re talking about a fundamentally different way of understanding and acting upon medical information.
So, what are the key ingredients in this intellectual stew?
- Machine Learning (ML): This is the workhorse of AI, teaching computers to identify patterns and make predictions based on data. Think of it as showing a computer a million pictures of cats so it can reliably identify a cat in the future. In clinical research, ML algorithms can sift through patient records to identify individuals at high risk for a particular disease.
- Deep Learning: A more sophisticated form of ML, deep learning uses artificial neural networks with multiple layers to analyze complex data with incredible accuracy. These networks, inspired by the structure of the human brain, are particularly adept at tasks like image recognition and natural language processing.
- Natural Language Processing (NLP): Medicine is awash in unstructured text – patient notes, research papers, clinical reports. NLP empowers computers to understand and extract meaningful information from this textual sea, unlocking insights that would otherwise remain buried.
- Generative AI: This is where things get really interesting. Generative AI can *create* new content, from simulating entire patient scenarios to designing novel drug molecules with specific properties. It’s like giving AI a blank canvas and asking it to paint a masterpiece of medical innovation.
- Predictive Analytics: By analyzing historical data, predictive analytics can forecast future outcomes, such as the likelihood of a clinical trial’s success or the potential for adverse drug reactions. It’s like having a crystal ball that offers glimpses into the future of patient health.
2. A Blast from the Past: How AI Got Its Lab Coat
The journey of AI into clinical research wasn’t an overnight sensation. It’s a story of gradual evolution, punctuated by moments of inspiration and driven by the relentless pursuit of knowledge.
- The Spark of an Idea (1950s-1970s): The seeds of AI were sown in the mid-20th century, with Alan Turing’s seminal question, “Can machines think?” igniting a firestorm of intellectual curiosity. The term “artificial intelligence” was soon coined, and early pioneers began exploring the possibilities of creating machines that could mimic human cognition. Early efforts in medical AI included diagnostic systems like INTERNIST-1, designed to diagnose complex diseases, and MYCIN, which recommended antibiotics. While these systems were rudimentary by today’s standards, they demonstrated the potential of AI to assist clinicians in decision-making.
- Learning to Learn (1980s-1990s): The introduction of machine learning and neural networks marked a turning point in AI’s development. These techniques allowed systems to learn from data without being explicitly programmed, opening up new possibilities for medical applications. The 1990s saw the emergence of AI in medical imaging, with systems capable of assisting radiologists in identifying abnormalities in X-rays and MRIs – a significant advance for early disease detection.
- Data Deluge to Deep Dive (2000s-Present): The explosion of data in the 21st century, coupled with breakthroughs in deep learning and NLP, propelled AI from theoretical promise to real-world impact. The 2010s witnessed the rise of personalized medicine, advanced imaging diagnostics (such as Google’s AI for diagnosing diabetic retinopathy), and virtual assistants. By the 2020s, AI was actively involved in designing new drugs – with the first AI-designed molecule entering human trials in 2020. Today, AI is being integrated across the entire clinical research journey, from optimizing trial design to predicting patient outcomes using “digital twins.”
3. The Current Pulse: What Everyone’s Saying About AI in Clinical Research
The integration of AI into clinical research has sparked a wide range of reactions, from enthusiastic embrace to cautious skepticism. It’s a complex landscape of hopes, fears, and expectations.
- Researchers: Excited but Cautious Optimists: Researchers see AI as a powerful tool for accelerating drug development, reducing costs, and improving the efficiency of clinical trials. They believe that generative AI can be a valuable assistant for tedious tasks and scenario planning. However, they also recognize the limitations of AI, including its lack of true creativity, the “black box” problem (where the reasoning behind an AI’s decision is opaque), and the potential for bias. Human oversight is seen as crucial to ensure the responsible use of AI in research.
- Clinicians: Helpful Assistant, Not a Replacement: Clinicians appreciate AI’s ability to assist with diagnoses, personalize treatment, monitor patients, and streamline workflows. They see AI as a way to free up their time to focus on direct patient care. However, they also have concerns about patient safety, the need for transparency in AI decision-making (“glass box” AI), the potential for “deskilling” of medical professionals, and the importance of maintaining the human touch in medicine. They emphasize that AI should augment, not replace, their clinical judgment.
- Regulators: Balancing Innovation and Safety: Regulatory bodies like the FDA and the EU face the challenge of fostering AI innovation while ensuring patient safety, ethical considerations, and data integrity. They are developing risk-based frameworks, demanding transparency and accountability, and requiring robust validation for high-impact AI tools. Compliance is paramount, and the regulatory landscape is still evolving.
4. The Elephant in the Room: Controversies and Challenges
The path to AI-powered clinical research is not without its obstacles. Several key challenges must be addressed to ensure the responsible and ethical implementation of AI in this field.
- Data Drama:
- Privacy Panic: Clinical data is highly sensitive, and protecting it from breaches and ensuring informed consent for its use (and reuse) are paramount. The potential for misuse of patient data raises serious ethical concerns.
- Bias Blunders: If the data used to train AI algorithms is biased (e.g., primarily from white male patients), the AI’s conclusions will also be biased, potentially exacerbating existing healthcare inequalities.
- Quality Control: The adage “garbage in, garbage out” applies to AI. Inconsistent, incomplete, or fragmented medical data can lead to unreliable AI models, undermining their accuracy and effectiveness.
- The “Black Box” Problem: When an AI system makes a recommendation but the reasoning behind that recommendation is opaque, it erodes trust and makes it difficult to validate the AI’s accuracy.
- Who’s to Blame? Determining accountability when an AI system makes an incorrect diagnosis or treatment suggestion is a complex ethical and legal challenge. Is the developer responsible? The clinician? The hospital?
- Loss of the Human Touch: Over-reliance on AI could lead to doctors missing subtle cues from patients or treating patients as mere data points. Empathy is not something that can be coded into an algorithm.
- Cost and Complexity: Implementing AI systems can be expensive and complex, requiring significant investments in infrastructure, training, and integration with existing workflows.
5. Crystal Ball Gazing: The Future of AI in Clinical Research
Despite the challenges, the future of AI in clinical research is bright. The potential benefits are too significant to ignore, and the field is poised for continued growth and innovation.
- Faster, Cheaper, Smarter Drug Development: AI is expected to continue accelerating the drug development process, reducing the time and cost of bringing new therapies to patients. Market growth in this area is predicted to skyrocket in the coming years.
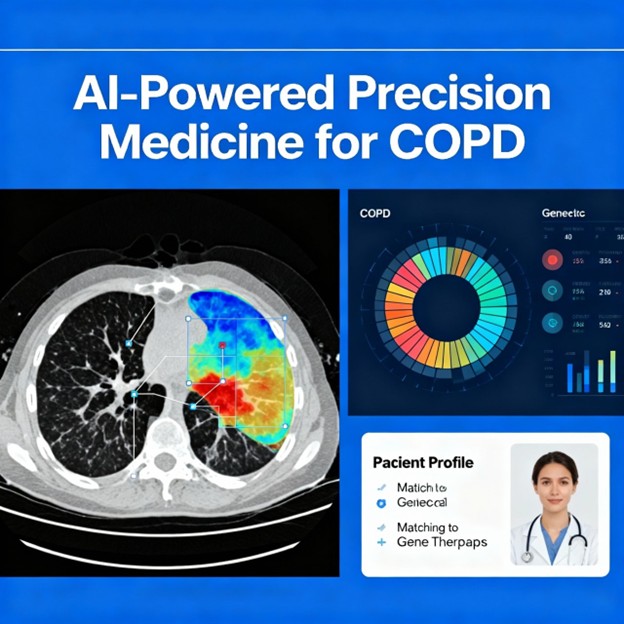
- Hyper-Personalized Medicine: AI will enable treatments to be tailored to an individual’s unique genetic makeup and health profile, ushering in an era of truly personalized medicine. AI algorithms will be able to analyze vast amounts of genomic and clinical data to identify optimal treatment strategies for each patient.
- Digital Twins for Everyone: Virtual replicas of patients could revolutionize clinical trials by reducing the need for large control groups and accelerating the testing of new therapies.
- Proactive Health Forecasting: AI may soon be able to predict an individual’s risk for a wide range of diseases years in advance, enabling proactive and preventive healthcare interventions.
- Regulatory Evolution: Regulatory agencies are expected to develop clearer and more standardized guidelines for AI in clinical research, with the FDA aiming to implement AI-assisted review tools by 2025.
- AI as an Indispensable Partner: AI will become an integral and essential part of the clinical research ecosystem, playing a crucial role in optimizing trial design, managing data, enhancing patient recruitment, and monitoring safety.
Conclusion
AI in clinical research is a transformative force with the potential to revolutionize healthcare. While challenges related to ethics, bias, and transparency must be addressed, the potential for accelerating breakthroughs, improving patient safety, and delivering truly personalized medicine is undeniable. The future of healthcare is intelligent, and it’s being built, one algorithm at a time. The question is not whether AI will transform clinical research, but how we can guide that transformation to ensure it benefits all of humanity.