The Science Behind Long COVID Brain Fog: How Japanese Researchers Unlocked the Mystery —and Lifestyle & Herbal Treatments to Manage It
Long COVID has emerged as one of the most perplexing medical challenges of our time, affecting millions of individuals worldwide with persistent symptoms that can last months or even years after initial COVID-19 infection. Among the most debilitating symptoms is brain fog—a frustrating cognitive impairment that leaves patients struggling with memory, concentration, and mental clarity. However, groundbreaking research from Japanese scientists has finally provided concrete answers about what causes this mysterious condition, opening new doors for both diagnosis and treatment.
What is Long COVID Brain Fog?
Long COVID, also known as Post-Acute Sequelae of SARS-CoV-2 infection (PASC), is a chronic condition that develops after the initial COVID-19 infection has resolved. According to the World Health Organization, approximately 6 in every 100 people who contract COVID-19 develop post-COVID-19 condition. However, recent comprehensive studies suggest the global prevalence may be as high as 36% among individuals with confirmed COVID-19 diagnosis.
Brain fog is a colloquial term used to describe a range of cognitive symptoms that affect a person’s ability to think clearly. It’s not an official medical diagnosis but rather describes a cluster of symptoms including:
- Difficulty concentrating and focusing
- Memory problems and forgetfulness
- Mental fatigue and sluggish thinking
- Trouble finding the right words
- Feeling “mentally cloudy” or confused
- Reduced processing speed
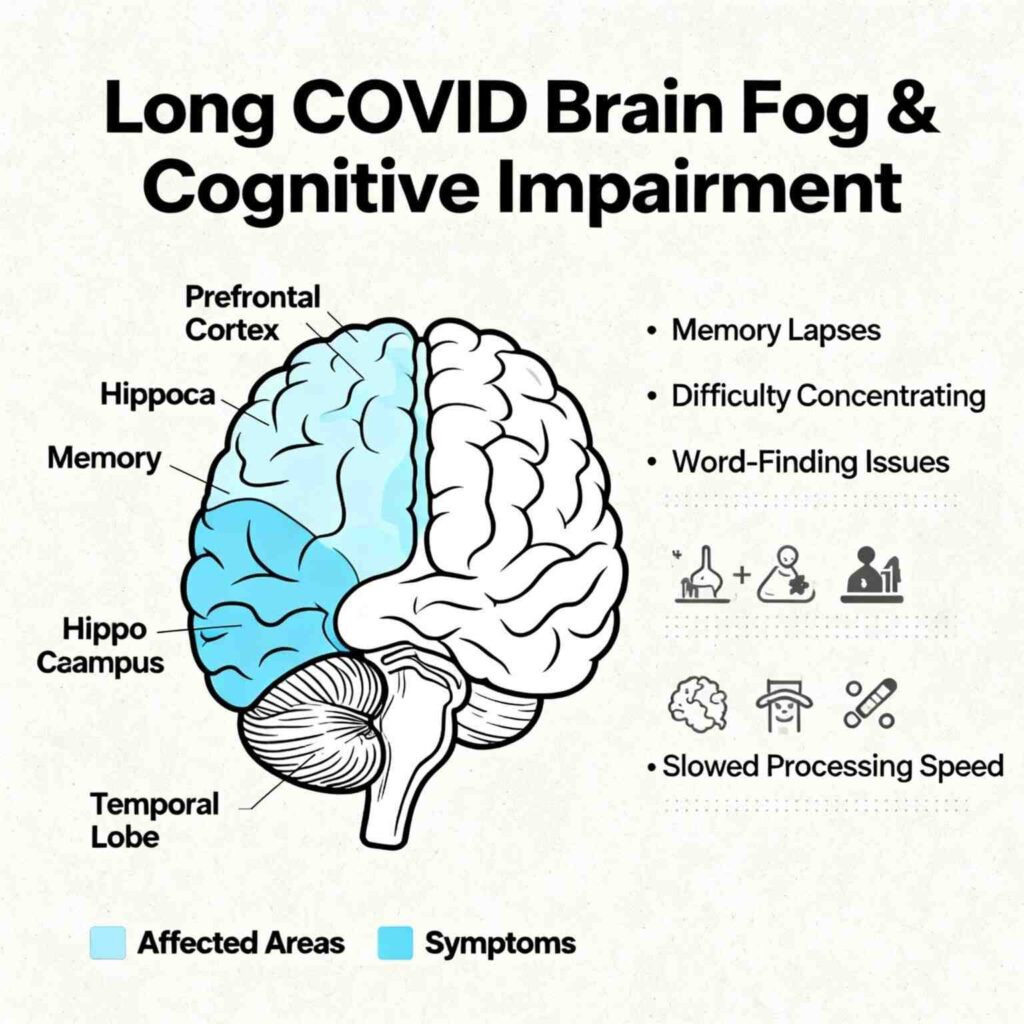
Medical illustration showing Long COVID brain fog symptoms
Brain fog affects over 80% of people with Long COVID, making it one of the most common and distressing symptoms of the condition. Unlike typical fatigue, brain fog specifically impacts cognitive function, making it difficult for patients to work, study, or perform daily activities that require mental effort.
The Breakthrough Discovery: AMPA Receptors Hold the Key
For years, scientists struggled to understand the biological mechanisms behind Long COVID brain fog. While imaging studies showed structural changes in the brain, they couldn’t pinpoint the specific molecular processes responsible for cognitive symptoms. This changed dramatically with the publication of groundbreaking research in Brain Communications on October 1, 2025, by Professor Takuya Takahashi and his team at Yokohama City University, Japan.
Understanding AMPA Receptors
To comprehend this discovery, we first need to understand AMPA receptors (AMPARs). These are specialized proteins found on the surface of brain cells (neurons) that play a crucial role in communication between brain cells. Think of them as molecular “receivers” that catch chemical messages called neurotransmitters.
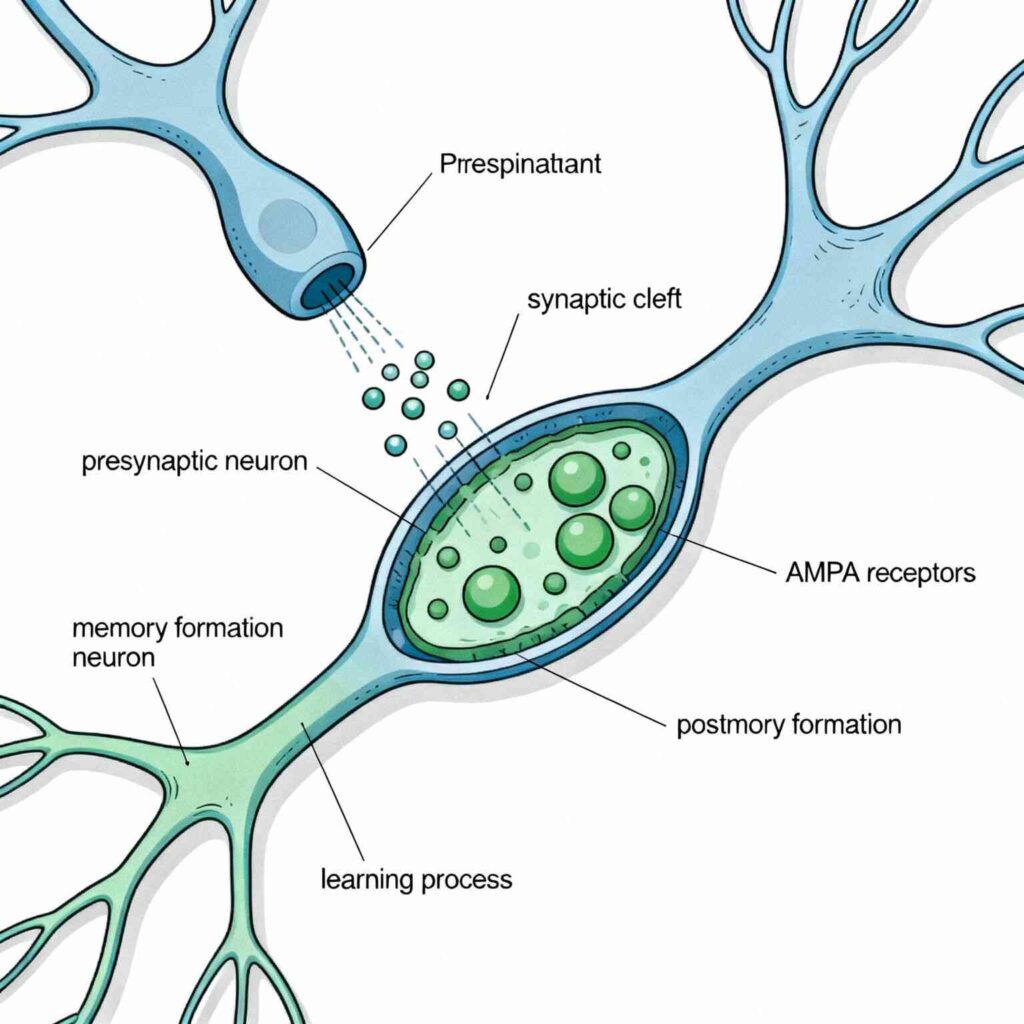
Scientific illustration of AMPA receptors at brain synapses
AMPA receptors are essential for:
- Fast brain communication: They enable rapid transmission of signals between neurons
- Learning and memory: They’re fundamental to how we form and recall memories
- Synaptic plasticity: They help strengthen or weaken connections between brain cells, which is the basis of learning
When the neurotransmitter glutamate (the brain’s primary excitatory chemical messenger) binds to AMPA receptors, it opens channels that allow sodium ions to flow into the neuron, creating an electrical signal that propagates through the brain.
The Revolutionary PET Imaging Technique
The Japanese research team developed an innovative brain imaging method called [11C]K-2 AMPAR PET imaging. This cutting-edge technique uses a special radioactive tracer that binds specifically to AMPA receptors, allowing scientists to visualize and measure their density in living human brains for the first time.
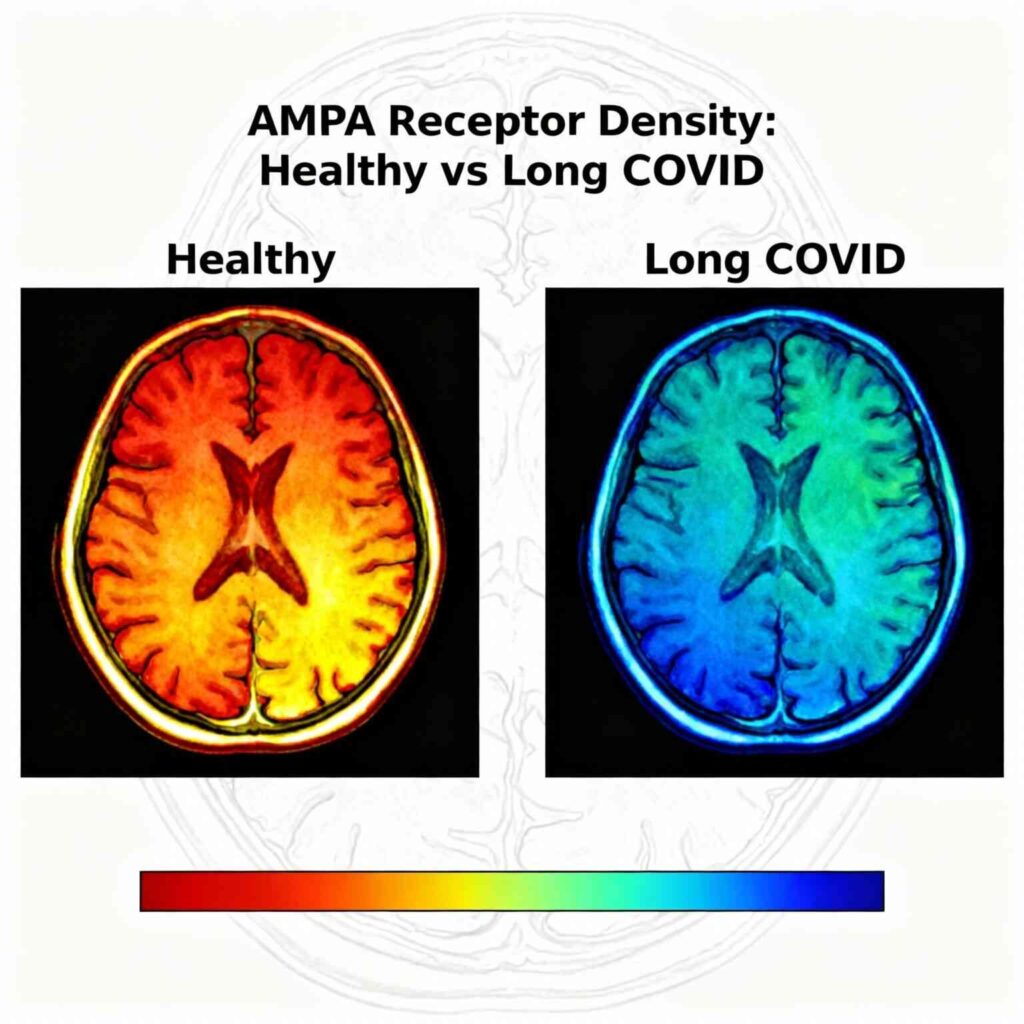
PET brain scan showing AMPA receptor density differences
The Shocking Results
When the researchers compared brain scans from 30 Long COVID patients with cognitive impairment to 80 healthy individuals, they made a remarkable discovery: Long COVID patients showed a widespread and significant increase in AMPA receptor density throughout their brains.
The key findings include:
- 100% sensitivity and 91% specificity: The imaging technique could distinguish Long COVID patients from healthy individuals with exceptional accuracy
- Direct correlation: The severity of AMPA receptor elevation directly matched the severity of cognitive symptoms
- Systemic involvement: The receptor changes weren’t limited to specific brain regions but occurred throughout the entire brain
- Inflammatory connection: Elevated AMPA receptor levels correlated with increased inflammatory markers in the blood
The Science Behind the Symptoms
How Normal Brain Function Works
Under normal circumstances, AMPA receptors are carefully regulated to maintain optimal brain function. They undergo constant trafficking—moving to and from the cell surface in a balanced dance that supports learning, memory, and cognitive processing.
During Long-Term Potentiation (LTP), which is the biological basis of learning and memory, AMPA receptors are recruited to synapses to strengthen connections between neurons. Conversely, during Long-Term Depression (LTD), receptors are removed from synapses to weaken unnecessary connections.
What Goes Wrong in Long COVID
In Long COVID brain fog, this delicate balance is disrupted. The research suggests that SARS-CoV-2 infection triggers a cascade of inflammatory responses that leads to:
- Excessive AMPA receptor trafficking: Too many receptors are moved to the cell surface
- Reduced receptor removal: The normal process of removing excess receptors (endocytosis) is impaired
- Inflammatory dysregulation: Immune system molecules like TNF-α and CCL2 abnormally promote receptor trafficking
This results in receptor hyperexpression—essentially, the brain’s communication system becomes overwhelmed with too many “receivers,” leading to:
- Information overload and misprocessing
- Difficulty filtering relevant from irrelevant information
- Cognitive fatigue as the brain works harder to process normal tasks
- Memory and attention problems
Impact on Daily Life and Consequences
Personal and Professional Impact
Long COVID brain fog can be devastating for patients, affecting every aspect of their lives. Common experiences include:
Work-related challenges:
- Inability to multitask effectively
- Difficulty completing complex projects
- Reduced productivity and job performance
- Some patients are forced to change careers or reduce working hours
Educational difficulties:
- Problems concentrating during lectures or studying
- Difficulty retaining new information
- Challenges with test-taking and academic performance
Daily living impacts:
- Forgetting appointments or important tasks
- Difficulty following conversations
- Problems with decision-making
- Increased mental fatigue from routine activities
Psychological and Social Consequences
The cognitive symptoms often lead to secondary problems:
- Depression and anxiety: Patients frequently develop mood disorders related to their cognitive limitations
- Social isolation: Difficulty participating in conversations and activities leads to withdrawal
- Loss of identity: Many patients report feeling like they’ve lost their former selves
- Medical skepticism: Before this research, many patients struggled to have their symptoms validated by healthcare providers
Economic Burden
Long COVID brain fog represents a significant economic challenge:
- Reduced workforce participation among affected individuals
- Increased healthcare utilization as patients seek answers and treatment
- Lost productivity estimated to affect millions globally
Current Research Findings and Global Statistics
Prevalence and Demographics
Recent comprehensive studies reveal the scope of Long COVID’s impact:
- Global prevalence: 36% of people with confirmed COVID-19 develop Long COVID symptoms
- Brain fog prevalence: Over 80% of Long COVID patients experience cognitive symptoms
- Persistence: Symptoms can last 1-2 years or longer, with 47% of patients still affected at 1-2 year follow-up
- Geographic variation: South America shows the highest prevalence at 51%
Risk Factors
Research has identified several key risk factors for developing Long COVID brain fog:
- Vaccination status: Unvaccinated individuals have 2.09 times higher risk
- Viral variant: Pre-Omicron infections carry 1.74 times higher risk
- Gender: Females have 1.56 times higher risk
- Age: Older adults and those with pre-existing conditions face higher risk
- Severity of initial infection: More severe acute COVID-19 correlates with worse long-term cognitive outcomes
Symptom Subtypes
Among Long COVID patients, the most common symptom categories are:
- Respiratory symptoms: 20%
- General fatigue: 20%
- Psychological symptoms: 18%
- Neurological symptoms (including brain fog): 16%
- Other systems also affected in smaller percentages
Treatment Developments and Future Prospects
AMPAR-Targeted Therapies
The discovery of AMPA receptor hyperexpression has opened new therapeutic avenues:
AMPAR Antagonists: Drugs that can suppress excessive AMPA receptor activity are being investigated as potential treatments. These medications could help normalize the overwhelming brain signaling that contributes to cognitive symptoms.
Precision Medicine Approach: The ability to measure AMPA receptor density with PET imaging could enable personalized treatment strategies, allowing doctors to:
- Confirm Long COVID brain fog diagnosis objectively
- Monitor treatment response over time
- Adjust medications based on individual receptor levels
Current Clinical Trials
Several treatment approaches are being studied in clinical trials:
Antiviral Medications:
- Nirmatrelvir-ritonavir (Paxlovid) is being tested in controlled trials for established Long COVID
- Other antivirals like molnupiravir and remdesivir are under investigation
Immune Modulators:
- Low-dose naltrexone has shown promise in open-label studies
- Anti-inflammatory approaches targeting the inflammatory cascade
Symptom-Specific Treatments:
- Cognitive rehabilitation programs
- Medications targeting specific neurotransmitter systems
Lifestyle Changes and Management Strategies
While awaiting targeted treatments, several lifestyle modifications can help manage brain fog symptoms:
Cognitive Strategies
Pacing and Energy Management:
- Break complex tasks into smaller, manageable steps
- Take frequent breaks during mentally demanding activities
- Prioritize important tasks during peak energy periods
Memory Aids:
- Use calendars, reminders, and note-taking systems
- Create structured routines to reduce cognitive load
- Employ external memory aids like smartphone apps
Sleep Optimization
Quality sleep is crucial for cognitive recovery:
- Maintain consistent sleep-wake cycles
- Aim for 7-9 hours of sleep nightly
- Create a sleep-friendly environment (cool, dark, quiet)
- Consider natural sleep aids like chamomile tea or melatonin under medical supervision
Physical Activity
Gentle Exercise:
- Light to moderate exercise can improve blood flow to the brain
- Start with 10-20 minute walks and gradually increase
- Yoga and stretching can help without overwhelming the system
- Avoid intense exercise that may worsen symptoms
Stress Management
Stress Reduction Techniques:
- Meditation and mindfulness practices
- Deep breathing exercises
- Progressive muscle relaxation
- Limit stressful activities when possible
Dietary Approaches and Brain Health
Nutritionally Dense Diet
- Omega-3 fatty acids: Found in fatty fish (salmon, sardines), walnuts, and chia seeds
- Antioxidant-rich foods: Berries, leafy greens, and colorful vegetables
- Whole grains: Provide steady glucose for brain energy
- Lean proteins: Support neurotransmitter production
Mediterranean and MIND Diets: These eating patterns emphasize foods that support brain health and may help reduce inflammation.
Foods to Limit
- Processed foods and refined sugars
- Trans fats and excessive saturated fats
- Excessive alcohol
- Foods high in additives and preservatives
Proper hydration is essential for cognitive function:
Hydration
- Aim for adequate daily water intake
- Even mild dehydration can worsen brain fog symptoms
- Monitor urine color as a hydration indicator
Natural and Herbal Treatment Options
Evidence-Based Natural Approaches
- Turmeric (Curcumin): Potent anti-inflammatory properties that may help reduce brain inflammation
- Ginger: May help with inflammation and circulation
- Green tea: Contains L-theanine and antioxidants that support brain function
- Ashwagandha: May help with stress response and cognitive function
- Rhodiola: Traditional use for mental fatigue and concentration
- Ginseng: May support cognitive performance and energy
Nutritional Supplements
Key Nutrients for Brain Health:
- Vitamin D: Deficiency linked to cognitive problems
- B-complex vitamins: Essential for neurotransmitter production
- Magnesium: Important for neural function and sleep
- Omega-3 supplements: If dietary intake is insufficient
- L-arginine plus Vitamin C: One study showed improvement in fatigue symptoms
- Probiotics: Support gut-brain axis health
- Coenzyme Q10: May support cellular energy production
Aromatherapy
Essential Oils for Cognitive Support:
- Peppermint: May improve alertness and concentration
- Rosemary: Traditional use for memory enhancement
- Lavender: May help with stress and sleep quality
- One clinical trial showed essential oil blends (clove, orange, frankincense, thyme) improved energy levels in Long COVID patients
Traditional Medicine Approaches
Traditional Chinese Medicine (TCM):
- Herbal formulations have shown promise in COVID-19 treatment
- Focus on restoring balance and supporting immune function
- May help regulate inflammation through gut-lung axis
Important Cautions:
- Always consult healthcare providers before starting herbal treatments
- Consider potential interactions with medications
- Quality and standardization of herbal products vary
- Some herbs may not be appropriate for all individuals
The Road Ahead: Hope for the Future
Validation and Recognition
The Japanese AMPA receptor research represents a watershed moment for Long COVID patients. For the first time, there is objective, measurable evidence of the biological basis of brain fog. This discovery:
- Validates patient experiences: Provides scientific proof that brain fog is a real, measurable condition
- Encourages medical recognition: May lead to better understanding and support from healthcare providers
- Accelerates research funding: Concrete targets may attract more research investment
Future Research Directions
Longitudinal Studies:
- Track AMPA receptor changes over time to understand recovery patterns
- Identify critical intervention windows for optimal treatment
Treatment Development:
- Design specific AMPAR-modulating medications
- Test combination therapies targeting multiple pathways
- Develop biomarker-guided treatment protocols
Diagnostic Applications:
- Standardize PET imaging protocols for clinical use
- Develop more accessible diagnostic methods
- Create treatment response monitoring systems
Broader Implications
This research extends beyond Long COVID, potentially informing understanding of:
- Other post-viral cognitive syndromes
- Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
- Age-related cognitive decline
- Inflammatory brain conditions
Conclusion: A New Chapter in Long COVID Understanding
The identification of AMPA receptor hyperexpression as the biological basis of Long COVID brain fog marks a revolutionary advancement in our understanding of this complex condition. This breakthrough transforms brain fog from a mysterious, subjective complaint into a measurable, targetable medical condition with clear biological mechanisms.
For the millions of individuals worldwide struggling with Long COVID brain fog, this research offers something that has been in short supply: hope. The discovery not only validates their experiences but also opens concrete pathways toward effective diagnosis and treatment. As Professor Takahashi noted, this work provides “a novel perspective and innovative solutions to the pressing medical challenge that is Long COVID”.
While we await the development of targeted AMPAR therapies, patients can take comfort in knowing that their symptoms have a real, measurable cause. Combined with the lifestyle modifications, natural approaches, and supportive treatments outlined above, this knowledge empowers both patients and healthcare providers to take a more informed, compassionate approach to managing Long COVID brain fog.
The journey from mystery to understanding has been long and challenging, but the destination—effective treatments that restore cognitive function and quality of life—is finally within sight. This research represents not just a scientific achievement, but a beacon of hope for millions of Long COVID patients worldwide who have been waiting for answers, validation, and most importantly, relief from their symptoms.