LLM-Powered Diagnostic Orchestrator Outperforms Doctors: Revolutionary Chain-of-Debate AI Achieves 4x Better Accuracy Than Physicians
The landscape of medical diagnosis is experiencing a seismic shift as large language models demonstrate diagnostic capabilities that substantially exceed human physician performance. Microsoft’s AI Diagnostic Orchestrator (MAI-DxO) achieved an unprecedented 85% accuracy rate on challenging diagnostic cases published in the New England Journal of Medicine, compared to just 20% average accuracy among 21 experienced physicians from the US and UK. This revolutionary system represents a fourfold improvement over average physician performance and marks the first time an AI system has demonstrated such dramatic superiority in complex clinical reasoning tasks. The breakthrough stems from an innovative “chain-of-debate” methodology that orchestrates multiple AI agents working collaboratively to analyze patient data, generate hypotheses, and debate diagnostic conclusions.

The Diagnostic Challenge in Modern Medicine
Medical diagnosis remains one of the most complex cognitive tasks in healthcare, requiring integration of vast amounts of clinical knowledge, pattern recognition, probabilistic reasoning, and systematic evaluation of competing hypotheses. Diagnostic errors affect an estimated 12 million Americans annually, contributing to significant morbidity, mortality, and healthcare costs. Traditional clinical decision support systems, while helpful, struggle with complex presentations requiring nuanced probabilistic reasoning and often fail to match the sophistication of human clinical judgment.
Limitations of Current AI Approaches
Previous AI diagnostic systems faced several critical limitations:
Single-Model Constraints: Traditional AI systems rely on individual models that lack the collaborative reasoning essential for complex diagnoses. These systems often produce narrow differential diagnoses and struggle with rare or atypical presentations.
Black Box Problem: Most AI diagnostic tools provide recommendations without transparent reasoning, making it difficult for physicians to understand, trust, or learn from AI suggestions.
Multiple-Choice Bias: Existing AI medical benchmarks primarily use standardized examination formats that test memorization rather than real-world clinical reasoning and sequential decision-making.
The Chain-of-Debate Revolution
Microsoft’s MAI-DxO introduces a fundamentally different approach that addresses these limitations through sophisticated multi-agent collaboration and transparent reasoning processes.
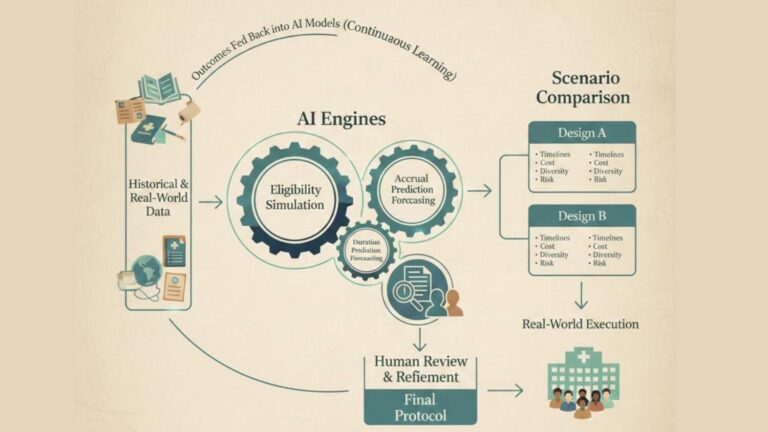
Orchestrated AI Collaboration
The system creates virtual panels of five AI agents, each with distinct specialized roles:
- Hypothesis Generator: Proposes initial diagnostic possibilities based on presenting symptoms
- Evidence Analyzer: Evaluates clinical data and test results to support or refute hypotheses
- Test Selector: Recommends diagnostic tests based on clinical reasoning and cost-effectiveness
- Debate Moderator: Coordinates discussion and ensures comprehensive evaluation
- Final Synthesizer: Integrates all perspectives to reach final diagnostic conclusions
This collaborative approach mimics real-world medical consultation, where multiple specialists contribute expertise to challenging cases, but operates at superhuman speed and with access to vast medical knowledge bases.
Sequential Diagnosis Methodology
Unlike traditional AI systems that provide instant answers, MAI-DxO employs sequential diagnosis that reflects authentic clinical workflows:
Progressive Information Integration: The system processes clinical information in stages, starting with chief complaints and physical examination findings, then incorporating laboratory results, imaging studies, and additional diagnostic tests as they become available.
Dynamic Hypothesis Refinement: AI agents continuously update their assessments as new information becomes available, demonstrating the iterative reasoning process essential for complex diagnoses.
Cost-Conscious Decision Making: The system is explicitly programmed to consider diagnostic test costs and can significantly reduce the number of tests required for accurate diagnosis, potentially saving hundreds of thousands of dollars in some cases.

Unprecedented Clinical Performance
Comparative Accuracy Studies
The most compelling evidence for LLM diagnostic superiority comes from rigorous head-to-head comparisons:
Microsoft MAI-DxO Study: 85% accuracy on New England Journal of Medicine cases vs. 20% for physicians represents the largest performance gap ever documented between AI and human diagnostic capabilities.
Specialized Neurology Study: A specialized LLM achieved 86.17% normalized score compared to 55.11% for practicing neurologists (p < 0.001) on complex neurological cases. For differential diagnosis questions, AI scored 85% vs. 46.15% for neurologists.
Gastroenterology Evaluation: Advanced LLMs achieved 76.1% accuracy in identifying correct diagnoses within their suggestions compared to 45.5% success rate for 22 experienced gastroenterologists on challenging GI cases.
Multi-Specialty Performance Analysis
A systematic review of 30 studies involving 19 different LLMs and 4,762 cases revealed impressive diagnostic capabilities across medical specialties:
Primary Diagnosis Accuracy: Ranged from 25% to 97.8% depending on model and clinical scenario, with best-performing models consistently achieving >90% accuracy on common presentations.
Triage Accuracy: Achieved 66.5% to 98% accuracy in determining appropriate levels of care and urgency.
Specialty-Specific Excellence: In ophthalmology, 77.8% of large models showed diagnostic accuracy comparable to healthcare professionals. GPT series LLMs achieved >80% diagnostic accuracy in multiple specialties, including general medicine, radiology, and emergency medicine.
Technical Architecture and Innovation
Advanced Natural Language Processing
Modern diagnostic LLMs leverage sophisticated architectures that process clinical information with unprecedented sophistication:
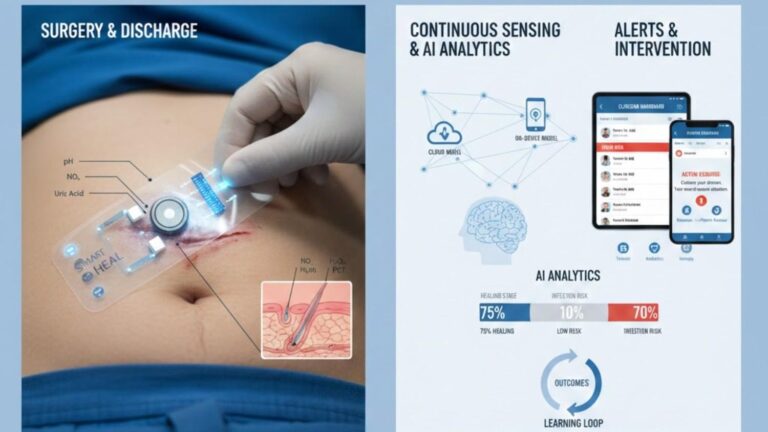
Multimodal Data Integration: Advanced systems combine textual clinical notes, laboratory values, imaging reports, and structured EHR data to create comprehensive patient assessments.
Contextual Understanding: LLMs demonstrate superior ability to understand medical terminology, clinical relationships, and temporal patterns in patient presentations.
Domain-Specific Training: Specialized medical LLMs fine-tuned on curated medical datasets show substantial improvements over general-purpose models in diagnostic accuracy and clinical relevance.
Explainable AI Integration
Modern diagnostic systems incorporate transparency features essential for clinical adoption:
Chain-of-Thought Reasoning: AI systems provide step-by-step explanations of their diagnostic reasoning, enabling physicians to follow and validate AI logic.
Evidence-Based Justification: Advanced systems cite specific clinical evidence supporting their diagnostic conclusions, enhancing physician confidence and enabling verification.
Uncertainty Quantification: Sophisticated models express confidence levels and identify areas of diagnostic uncertainty, supporting more nuanced clinical decision-making.
Real-World Clinical Integration
Electronic Health Record Analysis
LLMs excel at processing vast amounts of EHR data to identify diagnostic patterns invisible to human physicians:
Comprehensive Data Synthesis: AI systems can simultaneously analyze years of patient history, medication lists, laboratory trends, and imaging studies to identify subtle diagnostic clues.
Pattern Recognition: Machine learning algorithms detect complex relationships between clinical variables that may escape human attention, particularly in rare diseases or atypical presentations.
Temporal Analysis: LLMs track disease progression and treatment responses over time, providing insights into diagnostic evolution and therapeutic effectiveness.
Clinical Decision Support Enhancement
AI diagnostic systems are being integrated into clinical workflows as sophisticated decision support tools:
Differential Diagnosis Generation: LLMs consistently generate broader and more comprehensive differential diagnoses than human physicians, reducing the risk of missed diagnoses.
Risk Stratification: AI systems excel at identifying high-risk patients requiring immediate attention or specialized care.
Treatment Recommendation: Advanced systems provide evidence-based treatment suggestions aligned with current clinical guidelines and patient-specific factors.

Addressing Clinical Implementation Challenges
Human-AI Collaboration Optimization
Successful clinical integration requires careful attention to human-AI interaction dynamics:
Physician Training: Studies show that simply providing AI assistance doesn’t automatically improve physician performance. Effective integration requires training physicians to interpret and appropriately utilize AI recommendations.
Workflow Integration: AI systems must be seamlessly integrated into existing clinical workflows without disrupting efficiency or creating additional administrative burden.
Trust Building: Physician acceptance depends on transparency, reliability, and demonstrated clinical value rather than just raw accuracy metrics.
Quality Assurance and Safety
Clinical deployment requires robust safety and quality assurance frameworks:
Bias Mitigation: AI systems must be validated across diverse patient populations to ensure equitable performance and avoid perpetuating healthcare disparities.
Continuous Monitoring: Real-world performance must be continuously monitored to detect model drift, performance degradation, or systematic errors.
Regulatory Compliance: AI diagnostic systems must meet stringent regulatory requirements for safety, efficacy, and clinical utility before widespread deployment.
Specialized Applications and Success Stories
Emergency Medicine Integration
AI diagnostic systems show particular promise in emergency department settings:
Rapid Triage: AI systems can instantly analyze presenting symptoms, vital signs, and basic laboratory data to prioritize patient care and identify life-threatening conditions.
Rare Disease Detection: LLMs excel at identifying rare conditions that emergency physicians may encounter infrequently, reducing diagnostic delays and improving outcomes.
Resource Optimization: AI-guided diagnostic testing can reduce unnecessary procedures while ensuring appropriate care for high-risk patients.
Specialized Medical Domains
Different medical specialties show varying degrees of AI diagnostic success:
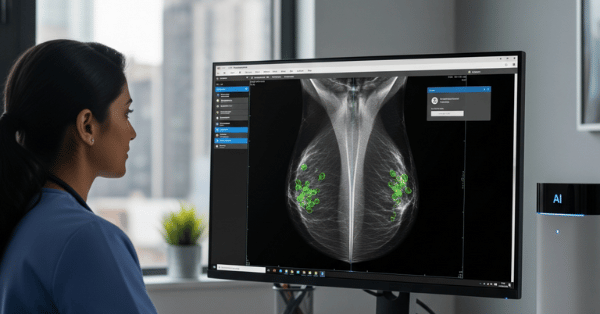
Radiology: AI systems achieve exceptional accuracy in image-based diagnoses, particularly for conditions with clear visual patterns.
Pathology: Digital pathology combined with AI enables rapid, accurate tissue diagnosis with performance often exceeding human pathologists.
Psychiatry: LLMs show promise in mental health diagnosis by analyzing speech patterns, behavioral descriptions, and clinical histories.
Economic Impact and Healthcare Transformation
Cost-Effectiveness Analysis
AI diagnostic systems offer substantial economic benefits:
Diagnostic Efficiency: Faster, more accurate diagnoses reduce healthcare costs through shorter hospital stays, fewer unnecessary tests, and improved treatment outcomes.
Resource Allocation: AI-guided triage and risk stratification enable more efficient allocation of healthcare resources and specialist referrals.
Error Reduction: Decreased diagnostic errors translate into reduced malpractice costs, fewer adverse events, and improved patient safety.
Global Healthcare Access
AI diagnostic systems could democratize access to expert-level medical diagnosis:
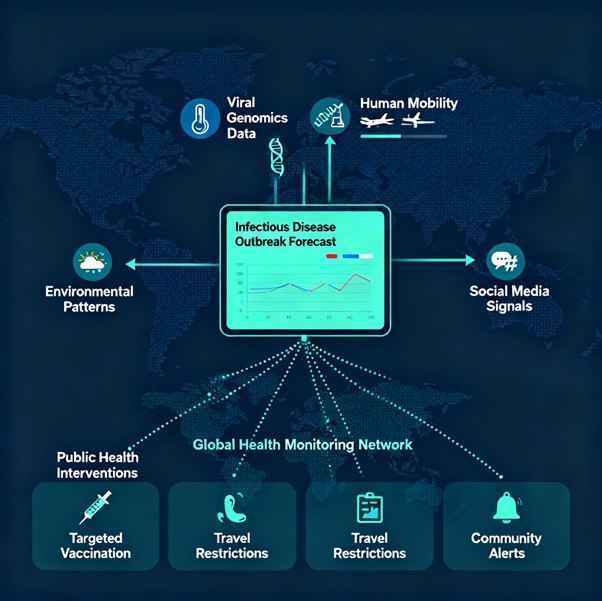
Underserved Populations: AI systems can provide sophisticated diagnostic capabilities in areas lacking specialist physicians.
Telemedicine Enhancement: Remote diagnostic AI can support primary care providers in delivering advanced diagnostic services.
Medical Education: AI systems serve as powerful teaching tools that expose medical trainees to rare cases and sophisticated diagnostic reasoning.
Future Directions and Innovation
Next-Generation Capabilities
Emerging developments promise even more sophisticated diagnostic AI:
Multimodal Integration: Future systems will seamlessly combine text, images, genomic data, and biosensor information for comprehensive diagnostic assessment.
Real-Time Learning: AI systems will continuously learn from new cases and outcomes, improving performance over time through federated learning approaches.
Personalized Medicine: AI diagnostics will integrate individual genetic, environmental, and lifestyle factors to provide highly personalized diagnostic and treatment recommendations.
Regulatory and Ethical Evolution
Successful implementation requires addressing complex regulatory and ethical challenges:
FDA Approval Pathways: New regulatory frameworks specifically designed for AI diagnostic systems are being developed to ensure safety while promoting innovation.
Liability Frameworks: Clear guidelines for responsibility and liability in AI-assisted diagnosis are essential for widespread clinical adoption.
Ethical Guidelines: Professional medical organizations must develop ethical standards for AI use in clinical diagnosis and decision-making.
Chain-of-Debate AI Diagnostic Process


Conclusion: The Dawn of AI-Augmented Medical Intelligence
The emergence of LLM-powered diagnostic orchestrators represents a transformative breakthrough in medical artificial intelligence that fundamentally challenges traditional assumptions about human diagnostic superiority. The documented 4x improvement in diagnostic accuracy over experienced physicians is not merely an incremental advance—it represents a quantum leap in clinical decision-making capability.
The chain-of-debate methodology pioneered by Microsoft’s MAI-DxO demonstrates that AI systems can replicate and exceed the collaborative reasoning processes that represent the pinnacle of human medical expertise. By orchestrating multiple specialized AI agents in transparent, sequential diagnostic workflows, these systems combine the benefits of artificial intelligence—vast knowledge, rapid processing, pattern recognition—with the collaborative wisdom traditionally exclusive to human medical teams.
The implications extend far beyond diagnostic accuracy improvements. These systems promise to democratize access to expert-level medical diagnosis, reduce healthcare costs through more efficient testing strategies, and serve as powerful educational tools that can expose physicians to rare cases and sophisticated diagnostic reasoning at an unprecedented scale.
However, realizing this potential requires thoughtful integration that preserves the essential human elements of medical care while harnessing AI’s superior analytical capabilities. The future of medicine lies not in replacing physicians with machines, but in creating human-AI partnerships that amplify clinical expertise and improve patient outcomes.
As regulatory frameworks evolve, clinical validation studies expand, and integration strategies mature, LLM-powered diagnostic orchestrators will increasingly become standard components of medical practice. This represents more than technological advancement—it is the beginning of a new era in which artificial intelligence and human expertise collaborate to achieve diagnostic accuracy and clinical outcomes that neither could accomplish alone.
The age of AI-augmented medical intelligence has arrived, and its impact on global healthcare will be profound, lasting, and transformative.