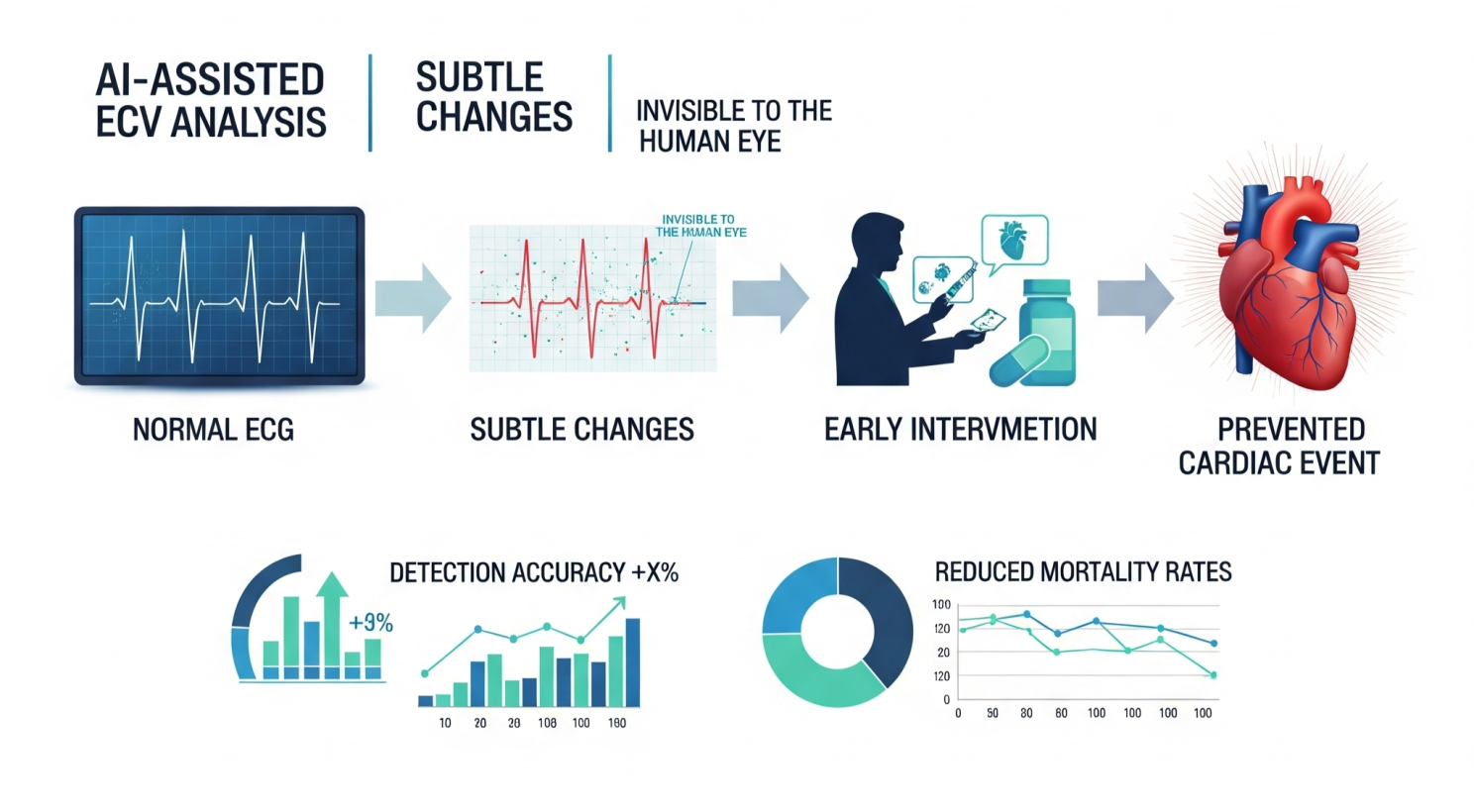
AI-Powered ECG Flags Silent Heart Disease: Revolutionary Early Warning System Predicts Cardiac Events Before Symptoms Emerge
The electrocardiogram, one of medicine’s most ubiquitous diagnostic tools, is undergoing a revolutionary transformation through artificial intelligence that promises to save millions of lives worldwide. Advanced machine learning algorithms can now detect subtle ECG patterns that predict life-threatening cardiac events days or even weeks before symptoms appear, achieving diagnostic accuracy that far surpasses human capabilities. A groundbreaking study involving over 240,000 ambulatory ECGs demonstrated that AI neural networks can identify patients at high risk for fatal arrhythmias up to two weeks in advance with over 70% accuracy and 99.9% specificity. This transformative capability represents a paradigm shift from reactive to predictive cardiac care, offering unprecedented opportunities for early intervention and prevention of sudden cardiac death.
The Silent Killer Challenge
Sudden cardiac death claims more than 5 million lives globally each year, often striking individuals with no prior diagnosis of heart disease. The tragic reality is that up to 50% of cardiac events occur without warning symptoms, leaving patients and healthcare providers with little opportunity for life-saving interventions. Traditional ECG interpretation, while valuable, relies on human pattern recognition that can miss subtle electrical changes indicating impending cardiac catastrophe.
The Limitations of Human ECG Interpretation
Conventional ECG analysis faces fundamental limitations that AI is uniquely positioned to overcome:
Pattern Complexity: The human heart generates intricate electrical patterns containing millions of data points per recording, far exceeding human cognitive capacity for comprehensive analysis.
Subtle Signal Detection: Critical changes indicating early disease may be so subtle they appear normal to trained cardiologists, yet contain predictive information detectable by sophisticated algorithms.
Subjective Variability: ECG interpretation varies significantly between clinicians, with studies showing substantial inter-observer disagreement even among experts.
Time Constraints: Emergency departments and clinical settings rarely allow the detailed analysis required to identify complex predictive patterns in ECG data.
Breakthrough AI Capabilities in Cardiac Prediction
Predicting Cardiac Arrest with Unprecedented Accuracy
The most compelling evidence of AI’s predictive power comes from a landmark study involving 47,505 ECGs from 25,672 patients that developed and validated a deep learning algorithm for predicting cardiac arrest within 24 hours. This revolutionary system achieved:
Performance Metrics:
- Area Under the Curve (AUROC): 0.913-0.948 across internal and external validation
- Sensitivity: 90% for high-risk identification
- Negative Predictive Value: >99.8%, providing exceptional reassurance for low-risk classifications
- External Validation: Maintained performance across different hospitals with varying patient populations
Extended Predictive Capability: The AI system’s high-risk classifications showed remarkable prognostic value beyond the immediate 24-hour window:
- 5.74% delayed cardiac arrest rate versus 0.33% in low-risk patients over 14 days
- 4.23% unexpected ICU transfer rate versus 0.82% in low-risk patients
- Significant hazard ratios for long-term adverse outcomes even after adjusting for clinical variables
Long-Range Arrhythmia Prediction
Recent advances have extended AI’s predictive horizon even further. A revolutionary study published in the European Heart Journal demonstrated that artificial neural networks analyzing 24-hour ambulatory ECGs can identify patients at risk for life-threatening arrhythmias up to two weeks in advance.
Key Breakthrough Findings:
- Analyzed several million hours of heartbeats from 240,000 ambulatory ECGs across six countries
- 70% accuracy in identifying patients who would experience dangerous arrhythmias within 14 days
- 99.9% specificity in correctly identifying low-risk patients
- Novel weak signals discovered that herald arrhythmia risk, focusing on ventricular electrical stimulation and relaxation timing
This capability represents a fundamental shift from reactive to predictive cardiology, enabling interventions days or weeks before life-threatening events occur.
Clinical Applications and Real-World Validation
Asymptomatic Left Ventricular Dysfunction Detection
One of AI-ECG’s most impactful applications involves detecting asymptomatic left ventricular dysfunction, a condition affecting 1.4-2.2% of the population that often goes undiagnosed until symptomatic heart failure develops.
Mayo Clinic’s Groundbreaking Research: A comprehensive study involving 97,829 patients with paired ECG and echocardiogram data demonstrated AI’s remarkable capability in identifying silent cardiac dysfunction:
- Area Under the Curve: 0.93, comparing favorably to cervical cytology (0.70) and mammography (0.85)
- 86.3% sensitivity and 85.7% specificity for detecting ejection fractions ≤35%
- 98.7% negative predictive value, providing exceptional reassurance for normal results
- Future-predictive capability: Among 1,335 false-positive cases, 147 developed LV dysfunction during follow-up, indicating fourfold higher risk compared to negative AI screens
Occlusion Myocardial Infarction (OMI) Detection
AI systems are revolutionizing heart attack diagnosis by identifying occlusion myocardial infarction in patients without classic ST-elevation patterns. A multi-site study involving 7,313 patients demonstrated AI’s superiority over human clinicians:
Performance Achievements:
- AUROC: 0.87 in external validation, significantly outperforming commercial systems (0.75) and practicing clinicians (0.80)
- 86% sensitivity and 98% specificity for OMI detection
- Enhanced rule-in and rule-out accuracy compared to HEART score
- Correctly reclassified one in three patients with chest pain when combined with clinical judgment
Clinical Impact: The AI system boosted sensitivity by 28 percentage points and precision by 32 percentage points compared to standard approaches, potentially preventing missed diagnoses that could prove fatal.
Single-Lead ECG Capabilities
Perhaps most remarkably, AI algorithms demonstrate exceptional performance using single-lead ECG data, making sophisticated cardiac screening accessible through wearable devices and portable monitors.
Wearable Device Integration: Research demonstrates that single-lead AI-ECG systems maintain diagnostic accuracy comparable to 12-lead systems:
- AUC: 0.87 for detecting atrial fibrillation using single-lead data
- 95.65% accuracy for heart disease classification from audio heart signals
- Continuous monitoring capability enabling real-time risk assessment through consumer wearables
Advanced AI Architectures and Technical Innovation
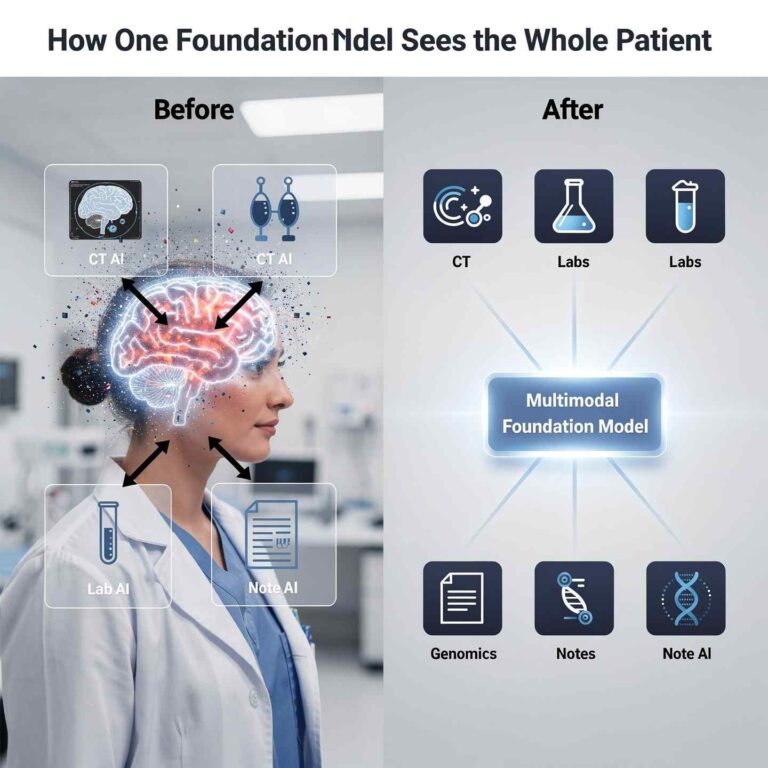
Multi-Modal Integration for Enhanced Accuracy
State-of-the-art AI systems combine ECG data with additional clinical information to achieve superior diagnostic performance:
Multimodal Deep Learning Architecture: Advanced systems integrate:
- Raw ECG waveform data processed through convolutional neural networks
- Patient demographics including age, sex, and clinical history
- Extended recording duration leveraging longer ECG segments for improved pattern recognition
Performance Improvements: Multimodal approaches achieve 92.1% AUROC and 87.4% accuracy for myocardial infarction detection, representing significant improvement over ECG-only models while addressing real-world clinical scenarios.
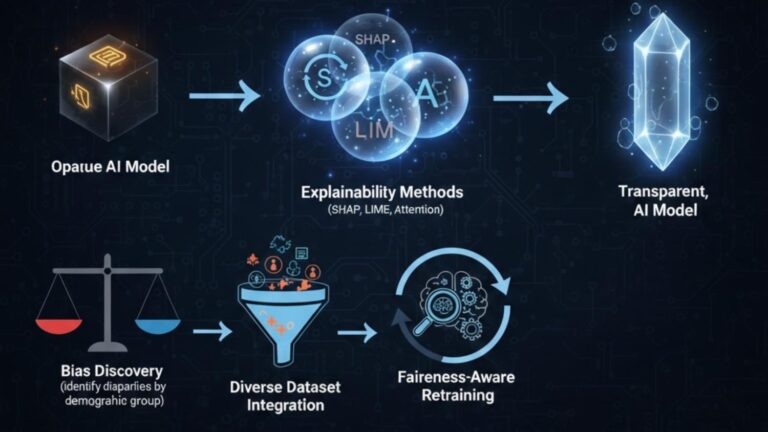
Explainable AI and Clinical Interpretation
Modern AI-ECG systems incorporate explainability features that enhance clinical adoption and trust:
Attention Mechanisms: Advanced models provide visual attention maps showing which ECG regions contribute most to diagnostic decisions.
Feature Identification: AI systems identify specific ECG characteristics driving predictions, including:
- QRS complex variations indicating electrical conduction abnormalities
- ST-segment changes too subtle for human detection
- T-wave morphology patterns reflecting repolarization abnormalities
- Heart rate variability metrics indicating autonomic dysfunction
Specialized Clinical Condition Detection
AI-ECG applications extend beyond cardiac arrest prediction to encompass comprehensive cardiovascular screening:
Structural Heart Disease Detection: The ADAPT-HEART model using over 99,000 paired ECG and echocardiogram records achieved >0.85 AUC for detecting six structural heart conditions including:
- Left ventricular systolic dysfunction
- Moderate or severe left-sided valvular disease
- Aortic stenosis and regurgitation
- Mitral regurgitation
- Left ventricular hypertrophy
Global Health Applications: AI-ECG algorithms demonstrate exceptional performance in resource-limited settings, with studies in Kenya showing 95.6% sensitivity and 79.4% specificity for heart failure detection compared to echocardiography.
Real-World Implementation and Clinical Integration
Emergency Department Integration
AI-ECG systems are being integrated into clinical workflows with demonstrated impact on patient outcomes:
Clinical Decision Support: Advanced systems provide real-time risk stratification that helps emergency physicians prioritize care:
- Automated high-risk alerts for patients requiring immediate intervention
- Risk scoring systems that complement clinical judgment
- Reduced diagnostic delays through rapid, objective analysis
Resource Optimization: AI systems help optimize healthcare resource allocation by:
- Identifying patients requiring cardiac catheterization with higher precision
- Reducing inappropriate activations of cardiac intervention teams
- Enabling faster triage in high-volume emergency departments
Remote Monitoring and Wearable Integration
The future of AI-ECG lies in continuous monitoring through wearable devices and remote monitoring systems:
Ambulatory Monitoring Enhancement: AI-enabled remote cardiac monitoring systems achieve:
- 96.67% detection rate for myocardial ischemia using AI-enhanced algorithms versus 86.67% with traditional monitoring
- Significant improvement in asymptomatic myocardial ischemia detection (P<0.01)
- Real-time alerting capability for healthcare providers
Consumer Device Integration: Advanced algorithms are being integrated into smartwatches and portable ECG devices, enabling:
- Population-scale screening for cardiac risk assessment
- Continuous monitoring of high-risk patients
- Early warning systems that can trigger immediate medical consultation
Addressing Implementation Challenges
Clinical Validation and Regulatory Considerations
Successful deployment of AI-ECG systems requires comprehensive validation across diverse populations:
Generalizability Assessment: Studies demonstrate consistent AI performance across:
- Different age groups, genders, and ethnicities
- Multiple healthcare systems and geographic regions
- Varying clinical settings from emergency departments to outpatient clinics
Regulatory Pathway: AI-ECG systems must undergo rigorous regulatory evaluation including:
- Clinical trial validation demonstrating improved patient outcomes
- Safety profile assessment ensuring no harm from false positives or negatives
- Integration testing with existing healthcare information systems
Physician Training and Adoption
Successful implementation requires comprehensive clinician education:
Interpretability Training: Healthcare providers need education on:
- Understanding AI predictions and confidence intervals
- Integrating AI insights with clinical judgment
- Recognizing limitations and appropriate use cases
Workflow Integration: Effective deployment requires seamless integration with existing clinical workflows without disrupting patient care efficiency.
Future Implications and Healthcare Transformation
Predictive Medicine Revolution
AI-ECG represents a cornerstone of predictive medicine that could fundamentally transform healthcare delivery:
Prevention-Focused Care: Early identification of cardiac risk enables:
- Preventive interventions before symptomatic disease develops
- Lifestyle modifications guided by objective risk assessment
- Pharmacological interventions to prevent disease progression
Population Health Impact: Widespread AI-ECG deployment could:
- Reduce sudden cardiac death through early identification and intervention
- Lower healthcare costs by preventing expensive emergency interventions
- Improve quality of life by maintaining cardiac health before symptoms develop
Global Health Democratization
AI-ECG technology offers unprecedented opportunities for global health equity:
Resource-Limited Settings: Single-lead AI algorithms enable sophisticated cardiac screening in areas lacking:
- Specialized cardiologists for ECG interpretation
- Advanced imaging equipment like echocardiography
- Complex laboratory testing for cardiac biomarkers
Scalable Screening Programs: AI enables population-scale cardiac screening that was previously impractical due to resource constraints.
AI-ECG Early Warning Timeline
Conclusion: The Future of Predictive Cardiology
AI-powered ECG analysis represents a transformative leap from reactive to predictive cardiovascular care. By detecting subtle electrical patterns that precede cardiac events by days or weeks, these systems offer unprecedented opportunities for life-saving early interventions.
The compelling clinical evidence demonstrates that AI can identify high-risk patients with remarkable accuracy while maintaining exceptional specificity to avoid unnecessary interventions. As these systems become integrated into routine clinical practice and consumer devices, they promise to democratize advanced cardiac screening and significantly reduce the global burden of sudden cardiac death.
The future of cardiology lies not in waiting for symptoms to appear, but in leveraging AI’s pattern recognition capabilities to identify and intervene before cardiac catastrophe strikes. This represents one of the most promising applications of artificial intelligence in healthcare—one that could save millions of lives while transforming our approach to cardiovascular disease prevention and management.
Through continued validation, regulatory approval, and clinical integration, AI-powered ECG systems will play an increasingly central role in creating a future where sudden cardiac death becomes preventable rather than inevitable.