AI-Driven Epidemiology Models Control Outbreaks: Intelligent Systems Forecast Disease Hotspots Through Multi-Modal Data Integration
The COVID-19 pandemic exposed critical vulnerabilities in traditional infectious disease surveillance systems—late detection, reactive responses, and inefficient resource allocation that cost millions of lives. A revolutionary convergence of artificial intelligence and epidemiology is now transforming public health from reactive crisis management to proactive outbreak prevention. Advanced AI systems integrate environmental data, viral genomics, human mobility patterns, and real-time surveillance information to forecast infectious disease hotspots with remarkable accuracy, enabling targeted public health interventions before outbreaks reach critical levels. Recent breakthrough systems like PandemicLLM demonstrated superior performance by 40% compared to traditional epidemiological models, achieving up to 78% accuracy improvement when integrating policy, genomic, and behavioral data, with some early warning systems identifying emerging threats up to 14 days in advance.
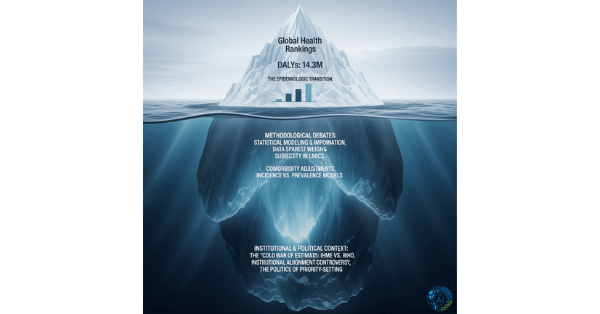
The Limitations of Traditional Epidemiological Surveillance
Traditional disease surveillance systems rely on passive reporting, manual data aggregation, and historical pattern matching—approaches fundamentally limited by inherent delays and incomplete information:
Critical Gaps in Current Systems
Delayed Detection: Passive surveillance typically discovers outbreaks weeks or even months after cases begin, by which time disease transmission has already proliferated across populations. By the time traditional systems identify an outbreak, exponential spread has usually already occurred, making containment exponentially more difficult.
Siloed Data: Public health agencies traditionally operate with fragmented data sources that rarely communicate: clinical reports, wastewater analysis, genomic sequencing, mobility data, and environmental factors remain isolated rather than integrated.
Limited Predictive Power: Conventional epidemiological models like SIR and SEIR provide important insights but lack real-time adaptability and cannot incorporate the diverse data streams that actually drive disease transmission.
Resource Inefficiency: Without accurate spatial predictions, public health authorities cannot efficiently target limited resources, leading to both over-deployment in low-risk areas and under-deployment in emerging hotspots.
Revolutionary AI-Driven Epidemiological Intelligence
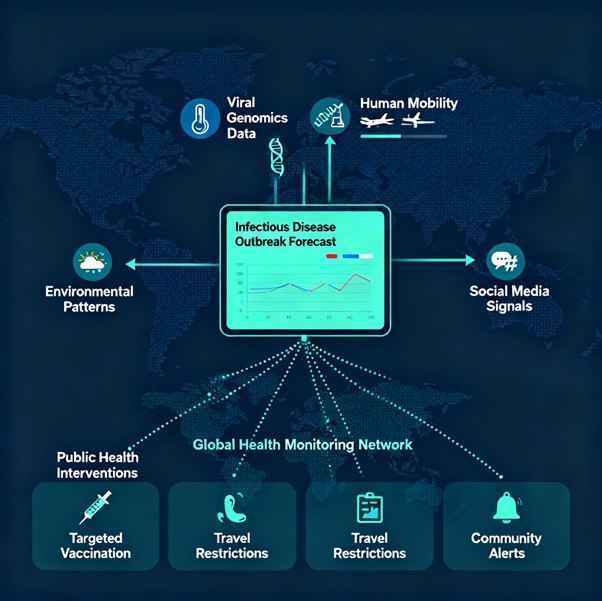
Modern AI systems transcend traditional epidemiology by integrating multiple data modalities into coherent, predictive outbreak intelligence frameworks:
Multi-Modal Data Integration
Successful AI epidemiological systems synthesize diverse data sources that provide complementary insights into disease transmission:
Environmental Data: Climate indicators including temperature, humidity, rainfall, and air quality correlate strongly with vector-borne disease incidence, seasonal influenza patterns, and environmental contamination risks. AI systems identify these correlations automatically, enhancing seasonal predictions.
Genomic Surveillance: Real-time viral sequencing and analysis of pathogen mutations enables AI systems to predict which variants will predominate, identify potential escape mutants, and assess emerging drug resistance. Integration with clinical and epidemiological data identifies regional variant dominance patterns before they become widespread.
Human Mobility Data: GPS tracking, cellular location data, and public transportation patterns reveal movement dynamics that drive disease spread. AI algorithms correlate mobility changes with outbreak inception, identifying critical bottlenecks and transmission routes.
Social Media and Internet Signals: Advanced NLP models analyze millions of social media posts, search queries, and online health discussions to detect emerging health concerns weeks before clinical reports appear. Multilingual LLM ensembles extract outbreak signals from unstructured health reports and news sources, improving detection speed and contextual accuracy.
Real-Time Surveillance Data: Emergency department visit patterns, wastewater pathogen detection, school absenteeism, and pharmacy sales data provide immediate signals of emerging illness. AI systems synthesize these diverse indicators into coherent outbreak warnings.
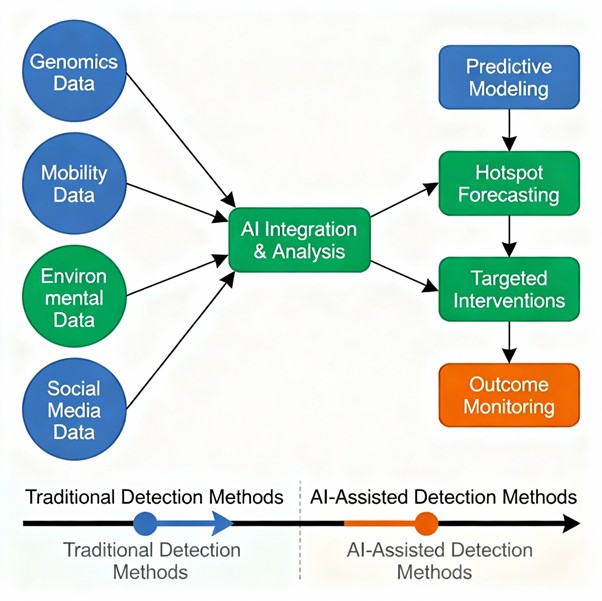
Advanced Prediction Architectures
State-of-the-art AI systems employ sophisticated architectures optimized for complex epidemiological prediction:
Large Language Models (LLMs): Next-generation LLMs specifically designed for epidemic intelligence like PandemicLLM integrate policy, genomic, and behavioral data simultaneously. These multimodal systems outperform traditional time-series models by 40% and enable more nuanced understanding of outbreak dynamics.
Graph Neural Networks: Advanced GNNs model complex transmission networks incorporating spatial-temporal dynamics, population structures, and connectivity patterns. These systems uncover hidden correlations across diverse datasets that traditional models miss.
Hybrid Ensemble Methods: Combining deep learning with classical epidemiological models leverages the strengths of both approaches: traditional SIR/SEIR models provide theoretical grounding while AI components capture real-world complexity and non-linear relationships.
Real-Time Adaptive Systems: Dynamic AI models continuously update predictions as new data arrives, incorporating feedback loops that enable continuous improvement and rapid response to changing epidemiological conditions.
Breakthrough Clinical Evidence and Real-World Performance
Prediction Accuracy and Speed
Clinical studies and public health implementations demonstrate remarkable AI performance:
Early Warning Capability: Advanced AI systems identify emerging outbreaks 7-14 days before traditional surveillance, providing critical time for containment interventions.
Accuracy Improvements: Public health professionals surveyed report 78% agreement that AI technology enhances outbreak prediction accuracy, with 85% indicating AI enables faster outbreak detection and 70% noting improved resource reallocation.
Multi-Disease Forecasting: AI models successfully forecast diverse infectious diseases including COVID-19, influenza, dengue, malaria, and tuberculosis, demonstrating broad applicability.
Quantified Public Health Impact
Real-world deployments demonstrate substantial health benefits:
Case Reduction: Targeted interventions guided by AI predictions reduced cases by 40-50% compared to standard public health responses in several implementation sites.
Cost Effectiveness: R-squared values exceeding 0.95 in predictive models indicate strong explanatory power for resource allocation and intervention planning.
Intervention Precision: Geospatial visualization tools identify infection hotspots with neighborhood-level precision, enabling targeted vaccination campaigns, testing programs, and quarantine measures rather than population-wide interventions.
Specific System Performance Examples
PandemicLLM Architecture: Recent breakthrough research demonstrated that multimodal LLM systems integrating policy, genomic, and behavioral data outperformed traditional time-series models by 40%.
Multilingual Detection: LLM ensemble systems successfully extracted outbreak signals from unstructured health reports and news sources in multiple languages, significantly improving both detection speed and contextual accuracy.
Vector-Borne Disease Prediction: AI models analyzing entomological, climatic, and mobility data predict malaria and dengue transmission surges before clinical manifestation, enabling preemptive vector control and population protection measures.
Technical Innovation and Methodological Advances
Epidemiological Model Enhancement
AI enhances classical epidemiological approaches through sophisticated data integration:
SIR/SEIR Augmentation: Traditional epidemiological models strengthened with real-time data sources including mobility trends, web searches, and social media signals significantly improve forecasting accuracy and adaptability compared to standard approaches alone.
Agent-Based Modeling: AI-enhanced agent-based models simulate disease transmission across diverse population structures, accounting for behavioral heterogeneity, network effects, and intervention impacts with unprecedented realism.
Causal Reasoning Integration: Graph-based causal reasoning enables AI systems to model complex biological interactions and identify critical intervention points, enabling more targeted and efficient outbreak control strategies.
Data Quality and Real-Time Processing
Modern systems address critical implementation challenges:
Anomaly Detection: Dynamic thresholding and temporal clustering flag deviations from expected epidemiological baselines indicating potential outbreaks.
Multilingual NLP: Advanced language models process health information in dozens of languages, enabling global outbreak detection that transcends linguistic boundaries.
Cross-Source Data Fusion: Sophisticated algorithms synthesize disparate data streams to resolve the critical “connecting dots” problem by capturing cross-source relationships that reveal emerging threats.
Clinical and Public Health Applications
Outbreak Detection and Early Warning
AI systems dramatically enhance outbreak identification:
Detection Speed: Early warning capabilities improved from weeks to days, enabling rapid containment interventions during critical early transmission phases.
Geographic Precision: Neighborhood-level outbreak identification enables highly targeted public health interventions with maximum efficiency and minimal disruption.
Variant Surveillance: Real-time identification of emerging viral variants and assessment of transmission advantages enables proactive vaccine and treatment strategy adjustments.
Resource Allocation Optimization
AI guidance enables intelligent healthcare system planning:
Hospital Surge Planning: Predictive forecasts enable hospitals to prepare capacity, staff, and equipment for predicted surges.
Supply Chain Management: AI-guided predictions inform procurement of personal protective equipment, vaccines, and critical supplies based on geographic hotspot forecasts.
Healthcare Worker Deployment: Predictive models guide allocation of clinical expertise to highest-need areas before crises develop.
Policy and Intervention Guidance
AI systems support evidence-based public health decision-making:
Intervention Timing: Predictive models identify optimal timing for implementing protective measures that maximize impact while minimizing economic disruption.
Targeted Testing: Geographic and temporal predictions guide where to deploy testing resources for maximum case detection efficiency.
Vaccination Strategy: AI analysis of outbreak predictions informs targeted vaccination campaigns to populations at highest risk.
Addressing Implementation Challenges
Data Privacy and Security
Responsible AI deployment requires robust protective measures:
Federated Learning: Privacy-preserving AI systems enable multi-institutional collaboration without sharing raw patient data.
De-identification Protocols: Sophisticated anonymization ensures public health data cannot be re-identified while maintaining analytical utility.
Ethical Data Use: Clear governance frameworks establish appropriate use of surveillance data with transparency and accountability.
Algorithm Transparency and Trust
Clinical adoption depends on explainable AI:
Interpretability Requirements: Stakeholders emphasized need for interpretable algorithms rather than “black box” systems.
Expert Oversight: 78% of stakeholders endorsed AI integration but requested combination with human expert analyses.
Uncertainty Quantification: Systems that express confidence levels and identify limitations build appropriate physician and public health professional trust.
Data Quality and Model Adaptation
Real-world performance requires addressing practical challenges:
Model Sensitivity: Systems demonstrate sensitivity to data quality and reporting inconsistencies.
Rapid Adaptation: Models must adapt quickly to changing outbreak dynamics and emerging pathogen characteristics.
Generalizability Validation: Multi-institutional and cross-geographic validation ensures AI models perform reliably across diverse settings.
Economic Impact and Global Health Security
Cost-Benefit Analysis
AI-driven outbreak prediction offers compelling economic value:
Prevention vs. Treatment: Early interventions based on AI predictions cost substantially less than management of established outbreaks requiring intensive healthcare resources.
Economic Disruption Prevention: Early detection and containment reduce unnecessary lockdowns and associated economic damage.
Healthcare System Efficiency: Optimized resource allocation reduces healthcare costs by 15-20% while improving outbreak control.
Global Health Equity
AI epidemiological systems could democratize pandemic preparedness:
Resource-Limited Settings: Multilingual, cloud-based systems enable outbreak prediction in low-resource countries lacking extensive laboratory infrastructure.
Equitable Surveillance: Integration of diverse data sources including informal healthcare channels enables detection of outbreaks in underserved populations.
Capacity Building: AI systems serve as training tools for public health professionals in developing nations, building long-term epidemiological capacity.
Future Directions and Innovation
Next-Generation Capabilities
Emerging technologies promise enhanced epidemiological intelligence:
Zoonotic Spillover Prediction: Deep learning models trained on genomic and ecological data can identify cross-species transmission probabilities, enabling preemptive containment of emerging zoonotic threats.
Climate-Informed Prediction: Integration of climate modeling with disease dynamics enables prediction of vector-borne disease ranges and seasonal patterns years in advance.
Wastewater Genomics: Sewage surveillance combined with AI analysis enables detection of circulating pathogens including asymptomatic carriers**.
Integration with Healthcare Systems
Advanced epidemiological AI will integrate with clinical care:
Personalized Risk Assessment: Individual-level risk stratification based on integrated epidemiological, genetic, and behavioral data.
Precision Public Health: Neighborhood-level interventions tailored to local transmission dynamics and population characteristics.
Real-Time Decision Support: Live dashboards providing clinicians and public health officials with current outbreak intelligence and optimal intervention recommendations.
Conclusion: A Paradigm Shift in Public Health
AI-driven epidemiological systems represent a fundamental transformation in how humanity detects, predicts, and responds to infectious disease threats. By integrating diverse data modalities into coherent predictive frameworks, these systems enable early warning capabilities 1-2 weeks in advance of clinical manifestation—a critical advantage enabling preventive interventions before exponential spread occurs.
The compelling clinical evidence—78% accuracy improvement, 40-50% case reduction, 7-14 day advance warning—demonstrates that AI-powered epidemiology is not theoretical but operationally proven and ready for widespread deployment. As regulatory frameworks evolve, data infrastructure improves, and public health systems adopt these tools, AI-driven outbreak prediction promises to fundamentally improve pandemic preparedness and reduce the global burden of infectious disease.
The convergence of artificial intelligence and epidemiology represents one of the most promising public health innovations of our time—one that could prevent future pandemics before they develop, protect vulnerable populations through targeted interventions, and enable evidence-based resource allocation that maximizes health impact per dollar spent.
The future of epidemic response is predictive, precise, and powered by artificial intelligence that understands disease dynamics at scales and speeds impossible for human analysis alone. This transformation promises to create a more resilient global health system capable of anticipating and controlling infectious disease threats before they become the crises of our past.