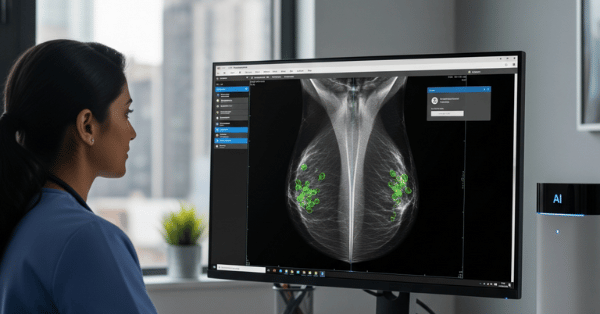
AI as Second Reader Boosts Breast Cancer Detection: Revolutionary Partnership Between Human Expertise and Machine Intelligence
Breast cancer screening has reached a transformative moment where artificial intelligence is proving to be the ideal “second reader” alongside human radiologists. A groundbreaking prospective study involving 24,543 women demonstrated that AI-assisted mammography screening achieved a 13.8% increase in cancer detection rates compared to traditional radiologist-only screening. This breakthrough represents one of the most significant advances in breast cancer detection accuracy in decades, offering hope for earlier detection and improved patient outcomes.
The Second Reader Revolution
Traditional breast cancer screening often employs double reading—where two radiologists independently examine mammograms—to improve detection accuracy. However, this approach faces significant challenges, including radiologist shortages, increased costs, and variable performance between readers. AI as a second reader offers a compelling solution that maintains or improves accuracy while dramatically reducing workload.
Landmark Clinical Evidence
South Korea’s AI-STREAM Study: The most comprehensive prospective evidence comes from South Korea’s national breast cancer screening program, where researchers directly compared radiologist performance with and without AI assistance in real-world conditions.
Key Results:
- Cancer Detection Rate: AI-assisted reading detected 140 cancers (5.70‰) versus 123 cancers (5.01‰) without AI – a 13.8% improvement (p < 0.001)
- Recall Rates: No significant difference in recall rates (4.53% with AI vs 4.48% without AI, p = 0.564)
- Positive Predictive Value: Higher with AI assistance (12.6 vs 11.2)
This study represents the first prospective evidence showing AI can increase breast cancer detection in an actual screening workflow rather than retrospective analysis.
Global Validation Across Healthcare Systems
European Multi-Center Validation: A comprehensive reader study involving 10 qualified radiologists across 5 reader pairs demonstrated that AI as a second reader improved sensitivity by 7.6% while reducing the workload by 71%—meaning most cases no longer required input from a human second reader.
Australian Population Study: Using Victoria’s mammography screening dataset, researchers simulated five AI-integrated pathways and found that AI as a second reader improved sensitivity by 1.9-2.5% and specificity by up to 0.6%, while reducing human reads by 48-80.7%.
Technical Performance Achievements
Superior Diagnostic Accuracy
Recent meta-analysis of 8 studies involving 120,950 patients revealed compelling performance differences:
AI Performance:
- Sensitivity: 0.85 (range 0.70-0.89)
- Specificity: 0.89
- Area Under Curve: 0.89
Radiologist Performance:
- Sensitivity: 0.77 (range 0.63-0.85)
- Specificity: 0.90
- Area Under Curve: 0.82
The data shows AI achieves higher sensitivity for cancer detection while maintaining comparable specificity, indicating fewer missed cancers without significantly more false positives.
Specialized Detection Capabilities
Interval Cancer Prevention: AI systems excel at identifying cancers that develop between routine screenings. UCLA researchers found that AI could potentially reduce interval breast cancers by 30% by flagging mammographically-visible tumors that radiologists missed. These are cancers visible on mammograms but not detected by human readers due to subtle signs or faint appearance.
Dense Breast Tissue Analysis: AI demonstrates particular strength in analyzing dense breast tissue, where traditional mammography faces significant challenges. Studies show AI maintains consistent performance across all breast density categories, unlike human readers whose accuracy can vary significantly with tissue density.
Real-Time Clinical Integration
Eye-Tracking Studies: Research using eye-tracking technology revealed that radiologists adjust their reading behavior when AI support is available. When AI provides low suspicion scores, radiologists move more efficiently through clearly normal cases. Conversely, high AI scores prompt more careful examination of challenging cases, effectively guiding attention to the most relevant regions.
Workflow Integration and Efficiency Gains
Dramatic Workload Reduction
50% Reading Volume Reduction: Multiple studies demonstrate that AI integration can reduce screen-reading volume by approximately 50% while maintaining or improving diagnostic accuracy. This includes reductions in arbitrations and stable or reduced recall rates.
Selective Application: Advanced AI systems can predict their own uncertainty, enabling selective use of AI support only when it provides meaningful benefit. This approach maximizes efficiency while minimizing potential errors.
Cost-Effectiveness Analysis
Short-term Cost Considerations: Initial implementation of AI in mammography screening increases costs compared to current double-reading practices. However, this must be balanced against long-term health gains and potential cost savings from earlier detection.
Resource Optimization: The dramatic reduction in human reading requirements enables broader screening coverage with existing radiologist resources, particularly valuable in regions with healthcare professional shortages.
Clinical Impact on Patient Outcomes
Early Detection Advantages
Prognostic Improvements: AI-assisted screening demonstrates particular effectiveness in detecting small-sized cancers (<20 mm), node-negative cases, low-grade invasive ductal carcinoma, and better prognostic luminal A subtype cancers. This suggests AI enhances early detection of cancers with favorable treatment outcomes.
Earlier Diagnosis Timeline: Long-term screening program analysis showed AI as a second reader could have led to earlier diagnosis in 24 patients, with an average of 29.92 ± 19.67 months earlier detection. Such early detection significantly improves treatment options and survival outcomes.
Specialized Population Benefits
High-Risk Patient Identification: AI systems effectively stratify patients for supplemental screening. Research shows AI can identify 84% of breast cancers in intermediate-risk populations (up to 50% lifetime risk) while requiring supplemental MRI for only 50% of examinations. This targeted approach optimizes resource utilization while maintaining high sensitivity.
Diverse Population Performance: Advanced AI models demonstrate consistent performance across mammography sites, machines, and diverse patient populations, addressing concerns about algorithmic bias and ensuring equitable healthcare delivery.
Addressing Clinical Challenges
Automation Bias Mitigation
Reader-Dependent Effects: Studies reveal that automation bias affects radiologists differently depending on their experience and the clinical setting. In single-reader environments, AI support improves performance, while in multi-reader settings, some degradation can occur if radiologists over-rely on AI recommendations.
Calibration Strategies: Successful AI implementation requires careful calibration to screening settings to ensure the AI’s sensitivity and specificity align with clinical objectives. Poorly calibrated AI can bias radiologist decisions in unintended directions.
Quality Assurance Frameworks
Continuous Monitoring: Clinical implementation demands robust monitoring of screening metrics to ensure desired impact. Performance indicators must be tracked continuously to identify and address any unintended consequences.
Training Requirements: Successful integration requires educating radiologists on critical interpretation of AI information to maintain accountability for clinical decisions. Radiologists must understand AI limitations and maintain independent clinical judgment.
Future Directions and Innovations
Advanced AI Architectures
Multi-Modal Integration: Next-generation AI systems combine imaging data with clinical information, genetic factors, and longitudinal health records to provide more comprehensive risk assessment and diagnostic support.
Explainable AI: Development of interpretable AI models that provide clear explanations for their decisions through attention maps and visualization techniques enhances radiologist trust and clinical adoption.
Personalized Screening Protocols
Risk-Based Screening: AI enables transition from age-based to risk-based screening protocols, particularly benefiting high-risk young women under 40 who typically aren’t routinely screened. This personalized approach optimizes screening frequency and modalities based on individual risk profiles.
Dynamic Risk Assessment: Advanced models measure changing risk levels over time, providing increasingly accurate predictions of future breast cancer development and enabling adaptive screening strategies.
AI Second Reader Performance Dashboard

Global Implementation Readiness
The convergence of strong clinical evidence, technological maturity, and healthcare system needs positions AI-assisted mammography screening for widespread clinical adoption. The technology has demonstrated:
- Consistent performance improvements across diverse healthcare settings
- Significant workflow efficiency gains addressing radiologist shortage challenges
- Enhanced patient outcomes through improved early detection
- Economic viability despite initial implementation costs
As healthcare systems worldwide grapple with increasing screening demands and limited radiologist availability, AI as a second reader represents a practical, evidence-based solution that enhances human expertise rather than replacing it.
The future of breast cancer screening lies not in choosing between human intelligence and artificial intelligence, but in optimizing their collaboration to achieve the best possible outcomes for patients. This partnership between radiologists and AI systems promises to make high-quality breast cancer screening more accessible, accurate, and efficient for women worldwide.