Cancer Vaccine Breakthrough 2025: mRNA Technology vs. Universal Cure Claims — What Science Really Shows
Imagine waking up to headlines declaring that scientists have finally cracked the code on cancer—a universal vaccine that could prevent and cure all forms of the disease that has plagued humanity for centuries. Sounds too good to be true, right? Well, you’re not wrong to be skeptical, but you’re also not wrong to feel hopeful.
The world of cancer vaccine research is buzzing with genuine breakthroughs that are reshaping how we think about treating this complex disease. But amid the excitement, exaggerated claims and sensational headlines are creating confusion about what’s real and what’s simply wishful thinking. Let’s dive deep into the fascinating world of cancer vaccines to separate fact from fiction and understand what these advances really mean for patients and families affected by cancer.
When Hope Meets Hype: The Cancer Vaccine Landscape Today
Cancer has always been humanity’s most formidable medical opponent. Despite decades of research and billions in funding, it remains the second leading cause of death globally. So when news breaks about potential “universal cancer vaccines,” it’s no wonder that hope and skepticism collide in equal measure.
The truth is, we’re living through a genuinely exciting time in cancer vaccine research. The same mRNA technology that brought us COVID-19 vaccines in record time is now being turned against cancer with remarkable results. But here’s the catch—the reality is far more nuanced than the headlines suggest.
Cancer vaccines aren’t your typical vaccines. While traditional vaccines like those for measles or flu prevent infections, most cancer vaccines are therapeutic, meaning they’re designed to treat existing cancers by training your immune system to recognize and destroy cancer cells. Think of them as a personalized boot camp for your immune system, teaching it to become a more effective cancer fighter.
Understanding Cancer Vaccines: A New Paradigm in Treatment
Cancer vaccines represent a revolutionary approach to cancer treatment that harnesses the body’s own immune system to fight malignancies. Unlike traditional vaccines that prevent infectious diseases, most cancer vaccines are therapeutic—designed to treat existing cancers rather than prevent them.
Types of Cancer Vaccines
Cancer vaccines fall into two primary categories:
Preventive Cancer Vaccines: These target cancer-causing viruses and are already in clinical use:
- HPV vaccines (Gardasil, Cervarix): Prevent cervical, anal, and other cancers caused by human papillomavirus
- Hepatitis B vaccine: Prevents liver cancer caused by chronic hepatitis B infection
Therapeutic Cancer Vaccines: These treat existing cancers by stimulating immune responses against tumor cells:
- Personalized mRNA vaccines: Tailored to individual tumor genetic profiles
- Neoantigen vaccines: Target tumor-specific mutated proteins
- Off-the-shelf vaccines: Standardized formulations targeting common cancer antigens
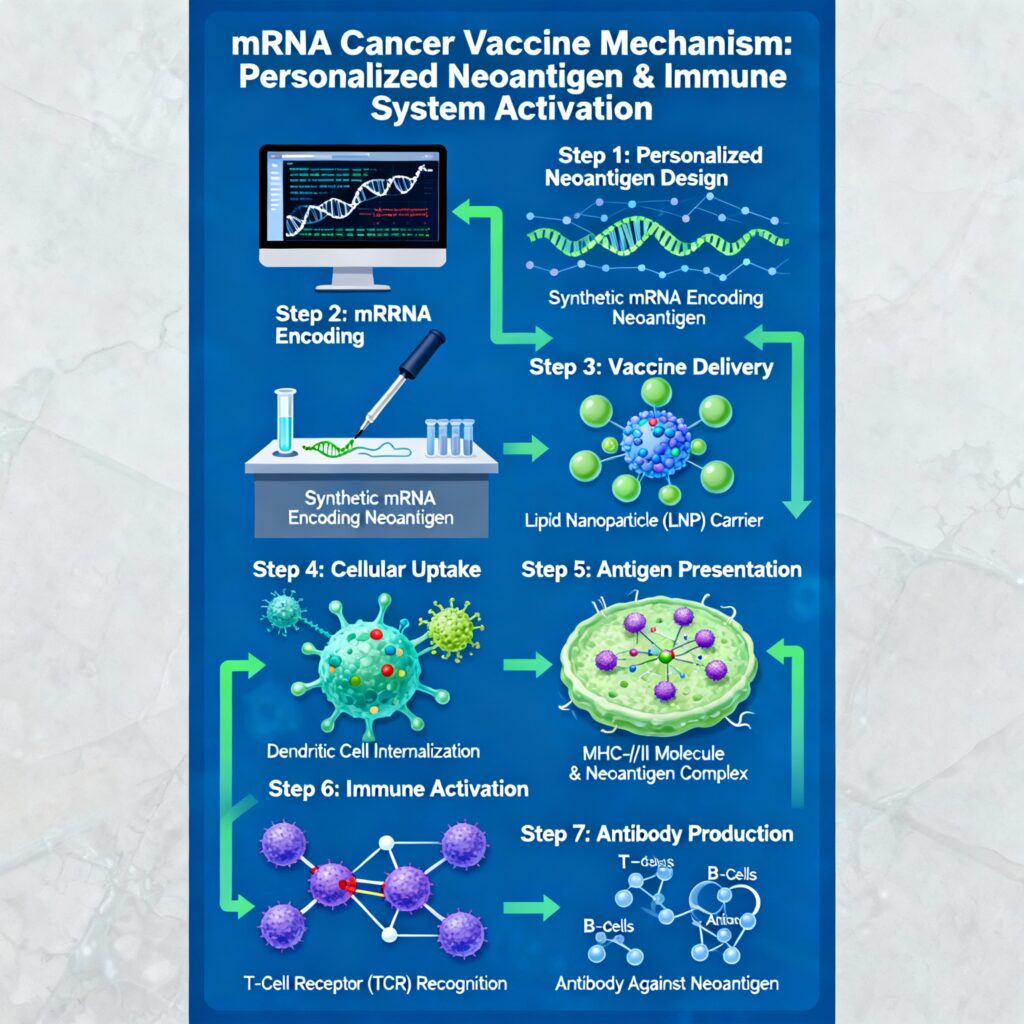
Scientific illustration of mRNA cancer vaccine mechanism and immune activation
The Science Behind the Promise: How Cancer Vaccines Actually Work
To understand why cancer vaccines represent such a breakthrough, we need to grasp why cancer is so difficult to treat in the first place. Cancer cells are essentially your own cells gone rogue—they’ve accumulated genetic mutations that make them grow uncontrollably and spread throughout the body. Because they originate from your own tissue, your immune system often doesn’t recognize them as threats.
This is where the genius of cancer vaccines comes in. Scientists have figured out how to identify the unique “fingerprints” that distinguish cancer cells from healthy cells. These fingerprints, called neoantigens, are like molecular name tags that only appear on cancer cells because of their specific mutations.
Here’s how the process works in simple terms:
Step 1: The Detective Work (Tumor Analysis)
Scientists analyze a piece of the patient’s tumor, sequencing its DNA to identify unique mutations (called neoantigens) that exist nowhere else in the patient’s body. It’s like creating a detailed criminal profile of the cancer.
Step 2: The Training Program (mRNA Design):
Using mRNA technology, they create a personalized vaccine that contains instructions for making these tumor-specific proteins. When injected into the patient, their cells follow these instructions and start producing the cancer proteins.
Step 3: The Immune Education (Immune Activation):
The patient’s immune system encounters these proteins and learns to recognize them as dangerous invaders. The mRNA instructs cells to produce these proteins, training the immune system to recognize and attack cancer cells. This training creates an army of specialized immune cells programmed to hunt down and destroy any cells displaying these specific cancer markers.
Step 4: The Long-term Memory (Memory Formation):
Just like with traditional vaccines, the immune system develops long-term memory cells that remain vigilant for years, ready to spring into action if the cancer tries to return.
Real Breakthroughs vs. Sensational Headlines
Now, let’s address the elephant in the room. You’ve probably seen headlines claiming that scientists have developed a “universal cancer vaccine” that’s 100% effective against all forms of cancer. These claims, while attention-grabbing, don’t match the scientific reality.
The Russia Enteromix Controversy: A Case Study in Medical Misinformation
Recent global headlines trumpeted Russia’s announcement of a “breakthrough” cancer vaccine called Enteromix, claiming 100% effectiveness against all cancers. The reality? This claim is based on a tiny study of just 48 patients, focuses primarily on colorectal cancer, and hasn’t undergone peer review—the gold standard for scientific validation.
Leading cancer researchers worldwide have emphasized that no cancer treatment currently provides 100% cure rates, and such claims should be viewed with extreme skepticism until supported by rigorous, independently verified data from large-scale trials.
The Real Breakthroughs: What’s Actually Working
While we debunk the hype, let’s celebrate the genuine progress that’s giving patients and families real reasons for hope.
The Moderna-Merck Success Story
One of the most compelling success stories comes from the collaboration between Moderna and Merck. Their personalized mRNA vaccine, called mRNA-4157, has shown remarkable results when combined with the immunotherapy drug pembrolizumab in melanoma patients.
The numbers are genuinely impressive: patients who received this combination therapy had a 49% reduction in their risk of cancer recurrence or death after three years of follow-up. Even more striking, they showed a 62% reduction in the risk of distant metastases—the spread of cancer to other parts of the body.
This wasn’t a small study either. The results were so promising that the FDA granted the combination “Breakthrough Therapy” designation, and a massive Phase III trial involving 1,100 patients is now underway globally.
BioNTech’s Pancreatic Cancer Victory
Pancreatic cancer is often called one of the most challenging cancers to treat, with historically poor survival rates. That’s why results from BioNTech’s personalized vaccine trial were so remarkable.
In their study, 50% of patients developed strong immune responses to the vaccine. But here’s the kicker—those patients who responded well had dramatically better outcomes. While patients who didn’t develop strong immune responses had a median relapse-free survival of just over three months, the responders hadn’t even reached their median survival time, meaning many were still cancer-free well beyond the typical prognosis.
UCLA’s Off-the-Shelf Innovation
Perhaps the most practical breakthrough comes from UCLA, where researchers developed an “off-the-shelf” vaccine called ELI-002 2P. Unlike personalized vaccines that take weeks to produce for each patient, this standardized vaccine targets common mutations found in many cancers.
The results speak for themselves: 84% of patients developed cancer-specific immune responses, with median survival times significantly exceeding historical expectations. Patients achieved a median relapse-free survival of 16.33 months and overall survival of 28.94 months—numbers that would have been considered impossible just a decade ago.
The Global Cancer Vaccine Revolution: Numbers That Matter
The excitement around cancer vaccines isn’t just academic—it’s translating into massive global investment and development efforts that suggest we’re on the cusp of a new era in cancer treatment.
The global cancer vaccine market is experiencing unprecedented growth, expanding from approximately $8.25-11.32 billion in 2024 to a projected $13.89-33.38 billion by 2029. This represents an annual growth rate of over 13%, reflecting both scientific confidence and commercial potential.
Currently, there are over 120 active clinical trials evaluating mRNA cancer vaccines worldwide, with more than 360 cancer vaccine candidates in various stages of development. Major pharmaceutical companies including BioNTech, Moderna, Merck, and Genentech are leading this charge, investing billions in research and development.
The timeline for bringing these treatments to market is becoming clearer. Moderna’s mRNA-4157 is expected to reach the market by 2028, while BioNTech’s pancreatic cancer vaccine is projected for launch by 2030. Multiple candidates are anticipated to receive their first commercial approvals by 2029.
Understanding the Challenge: Why Cancer Vaccines Are So Complex
To appreciate the magnitude of these breakthroughs, it’s essential to understand why developing effective cancer vaccines has been such a monumental challenge.
The Diversity Dilemma
Cancer isn’t a single disease—it’s actually hundreds of different diseases that happen to share some common characteristics. Even within a single tumor, different regions can contain genetically distinct cancer cells, creating a moving target that’s incredibly difficult to hit with any single treatment.
Think of it like trying to create a single key that can open hundreds of different locks, each with its own unique mechanism. This tumor heterogeneity is why the concept of a truly “universal” cancer vaccine remains elusive.
The Stealth Problem
Cancer cells have evolved sophisticated ways to hide from and disable the immune system. They can:
- Create a suppressive microenvironment around tumors that disables immune cells
- Stop producing the proteins that vaccines target, essentially changing their molecular disguise
- Activate immune “brake” systems that shut down anti-cancer responses
It’s like trying to fight an enemy that not only changes its appearance but also has the ability to turn your own weapons against you.
The Manufacturing Challenge
Creating personalized cancer vaccines presents unique logistical hurdles. Each vaccine must be individually designed and produced for a specific patient, taking 6-8 weeks from tumor analysis to final product. This process requires sophisticated laboratory capabilities and quality control measures that make treatment expensive and complex to scale.
What’s Available Now: The Current Treatment Reality
While we wait for the next generation of cancer vaccines, it’s important to understand what options exist today.
FDA-Approved Cancer Vaccines
Currently, only a handful of cancer vaccines have received regulatory approval:
For Prevention:
- Gardasil 9: Prevents cancers caused by human papillomavirus (HPV), including cervical, anal, and throat cancers
- Hepatitis B vaccines: Prevent liver cancer by protecting against chronic hepatitis B infection
For Treatment:
- Sipuleucel-T (Provenge): Approved for advanced prostate cancer
- Talimogene laherparepvec (T-VEC): Used for advanced melanoma
Breakthrough Designations and Fast-Track Approvals
Several promising candidates have received FDA Breakthrough Therapy designation, indicating that early evidence suggests they may offer substantial improvement over existing treatments:
- mRNA-4157: Currently in Phase III trials for melanoma
- Autogene cevumeran: Advancing toward Phase III trials for pancreatic cancer
- ELI-002 2P: In advanced trials for cancers with KRAS mutations
Living Your Best Life: Prevention and Lifestyle Strategies
While we eagerly await the next generation of cancer treatments, the most powerful tools for fighting cancer remain the lifestyle choices we make every day. The good news? These strategies are available to everyone right now, and they work.
The Foundation: Evidence-Based Prevention
Nutrition as Medicine
The foods you eat can be your first line of defense against cancer. Research consistently shows that certain dietary patterns significantly reduce cancer risk:
- Mediterranean-style eating: Rich in fruits, vegetables, whole grains, olive oil, and fish
- Colorful variety: Different colored fruits and vegetables provide unique protective compounds
- Fiber power: 25-35 grams daily from whole food sources support immune function and gut health
- Limit processed foods: Especially processed meats and foods high in added sugars
Movement Matters
Regular physical activity is one of the most powerful cancer prevention strategies available. The recommendations are straightforward but impactful:
- 150 minutes weekly of moderate-intensity exercise (like brisk walking)
- 2-3 strength training sessions per week
- Maintain healthy weight: BMI between 18.5-24.9
- Reduce sitting time: Take movement breaks throughout the day
Lifestyle Fundamentals
Several lifestyle factors dramatically impact cancer risk:
- Tobacco cessation: Eliminate all tobacco products—the single most important step for many cancer types
- Alcohol moderation: Follow recommended guidelines or avoid entirely
- Sun protection: Use sunscreen, protective clothing, and avoid peak sun hours
- Stress management: Chronic stress weakens immune surveillance of cancer cells
Sleep and Immune Function: The Overlooked Connection
Quality sleep is essential for optimal immune function, yet it’s often the first thing sacrificed in our busy lives. Your immune system does much of its cancer surveillance work while you sleep, making 7-9 hours of quality sleep not just beneficial but essential.
Create an optimal sleep environment by keeping your bedroom cool, dark, and quiet. Maintain consistent sleep and wake times, even on weekends, to support your body’s natural circadian rhythms that regulate immune function.
Natural Support: Evidence-Based Complementary Approaches
Many people want to know what natural approaches might support their cancer prevention efforts or complement conventional treatments. While it’s crucial to emphasize that no natural remedy can replace proven medical treatments, several evidence-based approaches show promise.
Anti-Inflammatory Powerhouses
Turmeric and Curcumin
This golden spice contains curcumin, a compound with potent anti-inflammatory properties. While most research has been done in laboratory settings, studies suggest curcumin may help reduce inflammation that contributes to cancer development.
Green Tea Benefits
Green tea contains epigallocatechin gallate (EGCG), an antioxidant compound that has shown anti-cancer properties in numerous studies. Drinking 2-3 cups daily may provide protective benefits.
Omega-3 Fatty Acids
Found in fatty fish, walnuts, and chia seeds, omega-3s help reduce inflammation throughout the body. If you don’t eat fish regularly, consider a high-quality fish oil supplement.
Immune-Supporting Nutrients
Several key nutrients play crucial roles in maintaining optimal immune function:
- Vitamin D: Often called the “sunshine vitamin,” adequate levels (30-50 ng/mL) are associated with better immune function and potentially lower cancer risk.
- Vitamin C: While megadoses aren’t necessary, ensuring adequate intake through fruits and vegetables supports immune cell function.
- Zinc: Essential for immune cell development and function. Found in oysters, beef, pumpkin seeds, and beans.
- Selenium: An antioxidant mineral that supports immune health. Brazil nuts are an excellent source.
Adaptogenic and Medicinal Herbs
- Ashwagandha: This adaptogenic herb may help the body manage stress and support immune function, though more human research is needed.
- Reishi Mushroom: Known as the “mushroom of immortality” in traditional Chinese medicine, reishi has been used for centuries to support immune function.
- Astragalus: Another traditional Chinese medicine herb used to support immune system function.
- Important Cautions: Always consult with healthcare providers before adding supplements, especially if you’re undergoing cancer treatment. Some natural compounds can interact with medications or interfere with treatments.
The Road Ahead: Realistic Timelines and Expectations
As we look toward the future of cancer vaccines, it’s important to maintain realistic expectations while acknowledging the genuine excitement surrounding current developments.
What’s Coming in the Next 5 Years (2025-2030)
- First Commercial Approvals: We can expect to see the first personalized mRNA cancer vaccines receive regulatory approval, likely starting with melanoma and expanding to other cancer types.
- Combination Becomes Standard: Cancer vaccines will increasingly be used alongside other immunotherapies like checkpoint inhibitors, creating more effective treatment protocols.
- Cost Reduction: As manufacturing processes improve and scale up, treatment costs should begin to decrease, making vaccines more accessible.
The Medium Term (2030-2035)
- Off-the-Shelf Options: Standardized vaccines targeting common cancer mutations will become available, eliminating the need for personalization in many cases.
- Prevention Applications: We may see vaccines developed for high-risk individuals, such as those with genetic predispositions to certain cancers.
- Expanded Applications: Successful vaccines will be tested and approved for additional cancer types.
Long-term Vision (2035 and Beyond)
- Routine Treatment: Cancer vaccines may become a standard part of cancer care, similar to how surgery, chemotherapy, and radiation are used today.
- Prevention Focus: The field may shift toward preventing cancer rather than just treating it.
- Global Access: Improvements in manufacturing and delivery should make these treatments available in low-resource settings worldwide.
Addressing Concerns: Safety, Side Effects, and Realistic Expectations
One of the most common questions about cancer vaccines concerns safety. The good news is that mRNA cancer vaccines have demonstrated excellent safety profiles in clinical trials, with most side effects being mild and temporary.
Common side effects typically include:
- Fatigue and mild flu-like symptoms
- Injection site reactions (pain, redness, swelling)
- Mild fever
- Muscle aches
These effects usually resolve within a few days and are actually signs that the immune system is responding to the vaccine.
Serious side effects have been rare in clinical trials, though researchers continue to monitor patients carefully for any unexpected reactions.
Managing Expectations
It’s crucial to understand that cancer vaccines, even when successful, are unlikely to be magic bullets. Instead, they’ll likely be most effective as part of comprehensive treatment approaches that may include:
- Surgery to remove tumors
- Chemotherapy or targeted therapy
- Radiation therapy
- Other immunotherapies
- Supportive care and lifestyle modifications
Response rates vary significantly between different cancer types and individual patients. Current data suggests that 15-30% of patients develop strong, lasting immune responses to personalized vaccines, though this percentage is expected to improve as the technology advances.
The Global Impact: Healthcare Equity and Access
As exciting as these developments are, we must address the elephant in the room: access and affordability. The current personalized approach to cancer vaccines is expensive and requires sophisticated laboratory infrastructure that isn’t available everywhere.
Challenges to Overcome
- Cost Barriers: Initial treatments are likely to be expensive, potentially limiting access to wealthy patients and nations.
- Infrastructure Requirements: Personalized vaccines require advanced laboratory capabilities for tumor sequencing and vaccine production.
- Geographic Disparities: Advanced treatments may initially be available only in major medical centers in developed countries.
Solutions in Development
- Technology Transfer: International efforts are underway to share manufacturing capabilities with developing nations.
- Standardized Approaches: Off-the-shelf vaccines that don’t require personalization will be much more accessible globally.
- Cost Reduction: As technology matures and scales up, costs should decrease significantly.
- International Cooperation: Global partnerships are working to ensure equitable access to breakthrough treatments.
Conclusion: Balancing Hope with Wisdom
As we stand at this remarkable moment in medical history, it’s natural to feel both excitement and impatience. The progress in cancer vaccine research is genuinely extraordinary, representing decades of scientific advancement converging into treatments that could transform how we approach cancer.
But perhaps the most important message is this: while we wait for these breakthrough treatments to become widely available, we’re not powerless. The lifestyle choices we make today—what we eat, how much we move, how well we sleep, how we manage stress—these remain our most potent weapons in the fight against cancer.
The future of cancer treatment is undoubtedly brighter than it’s ever been. mRNA cancer vaccines represent a new paradigm that harnesses our body’s own immune system to fight this ancient enemy. Clinical trials are showing remarkable results, major pharmaceutical companies are investing billions in development, and regulatory agencies are fast-tracking promising treatments.
Yet the most profound truth about cancer vaccines isn’t just their scientific elegance or commercial potential—it’s how they represent hope backed by rigorous science rather than empty promises. Unlike the sensational headlines claiming miraculous cures, the real breakthroughs in cancer vaccines are built on careful research, peer-reviewed data, and the incremental progress that characterizes genuine medical advancement.
For patients and families affected by cancer, this means staying informed through reputable sources, maintaining healthy skepticism about miracle cure claims, and working closely with healthcare teams to understand all available options. For those focused on prevention, it means embracing the lifestyle strategies we know work while staying hopeful about future possibilities.
The war against cancer isn’t over, but we’re winning more battles than ever before. And with cancer vaccines joining our arsenal, we have every reason to believe that the victories will keep coming. The key is maintaining our commitment to evidence-based medicine while never losing sight of the human hope that drives all medical progress.
In this exciting new chapter of cancer research, science and hope are finally working hand in hand to write a better ending to the cancer story. And that, more than any sensational headline, is truly cause for optimism.

