Smart Wearables Predict Flare-Ups in Chronic Illness: AI Analytics Forecast Respiratory Crises Days Before Symptoms Emerge
Chronic respiratory diseases like asthma and chronic obstructive pulmonary disease (COPD) affect over 500 million people worldwide, with acute exacerbations representing life-threatening emergencies that drive millions of costly hospital visits annually. Revolutionary advances in wearable technology combined with artificial intelligence are now enabling prediction of these dangerous flare-ups up to 48 hours before symptoms appear. A landmark study achieved 92.1% accuracy in predicting COPD exacerbations 7 days in advance using smartwatch data, while machine learning models for asthma reached 90% sensitivity in forecasting attacks 3 days early. This breakthrough technology promises to transform chronic disease management from reactive emergency care to proactive prevention, potentially saving thousands of lives and billions in healthcare costs.

The Hidden Crisis of Respiratory Exacerbations
Acute exacerbations of chronic respiratory diseases represent medical emergencies that can rapidly progress from manageable symptoms to life-threatening respiratory failure. COPD exacerbations alone result in over 2.2 million hospitalizations annually in the United States, while severe asthma attacks send nearly 2 million people to emergency departments each year.
The Prediction Challenge
Traditional approaches to managing chronic respiratory diseases rely on reactive treatment after symptoms have already worsened. By the time patients recognize serious symptoms, physiological changes have often progressed to dangerous levels requiring emergency intervention. The narrow window between early warning signs and acute crisis makes prediction extremely challenging using conventional monitoring methods.
Current limitations include:
- Subjective symptom reporting that varies between patients and may miss subtle early changes
- Intermittent clinical assessments that capture only snapshots of patient status
- Environmental trigger monitoring that relies on patient memory and self-reporting
- Medication adherence tracking that depends on patient honesty and recall
How AI-Powered Wearables Transform Prediction
Modern smartwatches and wearable devices continuously collect rich physiological and behavioral data that AI algorithms can analyze to detect subtle patterns preceding exacerbations:
Comprehensive Biometric Monitoring
Advanced wearable devices track multiple data streams that change in predictable ways before respiratory crises:
Activity Patterns: Daily steps, stairs climbed, and movement distance represent powerful predictors of impending exacerbations. Studies show these metrics often decrease 3-7 days before acute episodes as patients unconsciously reduce activity in response to early physiological changes.
Heart Rate Variability: Changes in heart rate patterns and variability reflect autonomic nervous system responses to respiratory stress, often appearing days before conscious symptoms.
Sleep Quality Metrics: Sleep duration, efficiency, and breathing patterns during sleep deteriorate before exacerbations as respiratory function declines.
Environmental Integration: Air quality sensors, pollen counts, and weather data combined with GPS location tracking provide contextual information about exposure to known triggers.
Breakthrough Clinical Evidence
COPD Exacerbation Prediction Success
The most compelling evidence comes from a comprehensive study involving 67 COPD patients monitored continuously over 4 months using wearable devices, smartphone apps, and home air quality sensors. The AI prediction system achieved remarkable performance:
Performance Metrics:
- 92.1% accuracy in predicting COPD exacerbations within 7 days
- 94% sensitivity ensuring very few actual exacerbations were missed
- 90.4% specificity minimizing false alarms that could cause unnecessary anxiety
- Area under the curve >0.9 demonstrating excellent discriminative ability
Key Predictive Features: The study identified daily steps walked, stairs climbed, and daily distance moved as the most important variables in the prediction model, highlighting how subtle changes in physical activity precede acute respiratory deterioration.
Asthma Attack Forecasting
Machine learning models for asthma prediction have demonstrated equally impressive capabilities:
Zhang et al. Study Results: AI models utilizing logistic regression achieved optimal balance of sensitivity and specificity for detecting asthma exacerbations:
- 90% sensitivity in detecting impending exacerbations
- 83% specificity in avoiding false positive predictions
- 3-day prediction window providing adequate time for preventive interventions
Peak Flow Integration: AI systems analyzing daily peak expiratory flow measurements combined with symptom data provide superior prediction accuracy compared to either data source alone.
Multi-Modal Prediction Systems
The most advanced prediction systems integrate multiple data sources for enhanced accuracy:
Environmental Data Integration: AI models combining physiological data with environmental factors including air quality, pollen counts, and weather patterns achieve 10-20% accuracy improvements over single-source approaches.
Digital Inhaler Data: Smart inhalers equipped with sensors tracking medication usage patterns provide additional predictive power, with studies showing reliable prediction of near-term COPD exacerbations based on rescue inhaler usage patterns.
Advanced AI Methodologies
Machine Learning Architectures
Modern prediction systems employ sophisticated AI architectures optimized for time-series medical data:
Deep Learning Models: Convolutional neural networks and recurrent neural networks excel at identifying complex temporal patterns in physiological data that precede exacerbations.
Ensemble Methods: Voting ensemble classifiers combining multiple algorithms achieve superior performance by leveraging the strengths of different machine learning approaches.
Real-Time Processing: Stream processing algorithms analyze continuous data feeds in real-time, enabling immediate alerts when exacerbation risk increases.
Personalized Risk Assessment
AI systems increasingly provide personalized predictions tailored to individual patient characteristics:
Risk Stratification: Machine learning models identify high-risk patients who benefit most from intensive monitoring and preventive interventions.
Trigger Identification: AI algorithms identify personalized trigger patterns unique to each patient, enabling targeted avoidance strategies.
Medication Optimization: Predictive systems recommend personalized medication adjustments based on individual response patterns and risk factors.
Clinical Implementation and Real-World Impact
Healthcare System Integration
Successful deployment of wearable-based prediction systems requires seamless integration with existing healthcare workflows:
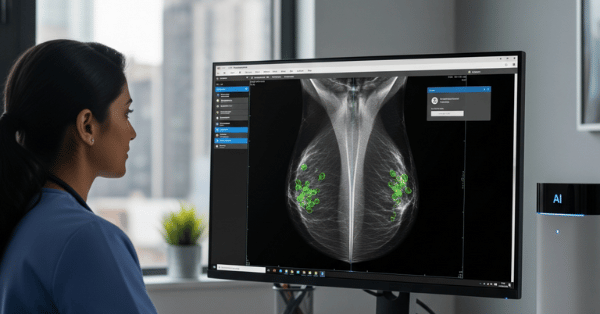
Clinical Decision Support: AI alerts integrate with electronic health records to provide clinicians with actionable insights during routine visits and emergency consultations.
Patient Engagement Platforms: Mobile apps provide patients with personalized risk scores and recommendations for preventive actions when exacerbation risk increases.
Telemedicine Integration: Remote monitoring capabilities enable proactive clinical interventions without requiring in-person visits, particularly valuable for patients with limited mobility or access to specialized care.
Emergency Department Impact
Predictive wearable systems demonstrate significant potential for reducing emergency healthcare utilization:
Early Intervention: 48-72 hour advance warning enables initiation of preventive treatments that can often prevent progression to emergency-level severity.
Resource Planning: Population-level prediction models help hospitals anticipate and prepare for increased respiratory emergency volumes during high-risk periods.
Cost Reduction: Prevention of emergency visits through early intervention results in substantial healthcare cost savings, with studies suggesting potential savings of $2,000-$5,000 per prevented hospitalization.
Addressing Implementation Challenges
Technical Validation and Reliability
Clinical deployment requires addressing several technical challenges:
Multi-Center Validation: Prediction models must demonstrate consistent performance across diverse patient populations and healthcare settings to ensure generalizability.
False Positive Management: Minimizing false alarms is crucial for maintaining patient confidence and preventing alert fatigue among healthcare providers.
Data Quality Assurance: Wearable device reliability and data completeness significantly impact prediction accuracy, requiring robust quality control measures.
Patient Adoption and Engagement
Successful implementation depends on patient acceptance and consistent device usage:
User Experience Design: Intuitive interfaces and clear communication about prediction rationale enhance patient understanding and engagement.
Privacy Protection: Robust data security measures address patient concerns about continuous health monitoring and data sharing.
Clinical Integration: Clear pathways for acting on predictions ensure patients and providers know how to respond effectively to alerts.
Economic Impact and Healthcare Transformation
Cost-Effectiveness Analysis
Wearable-based prediction systems offer compelling economic value:
Prevention vs. Treatment Costs: Early intervention medications and preventive measures cost significantly less than emergency department visits, hospitalizations, and intensive care treatment.
Healthcare Utilization Reduction: Studies suggest 20-30% reduction in emergency visits among patients using AI-powered prediction systems compared to standard care.
Productivity Benefits: Preventing severe exacerbations reduces work absences and disability claims, providing additional economic benefits beyond direct healthcare costs.
Population Health Applications
Large-scale deployment enables population-level health management:
Public Health Surveillance: Aggregated prediction data can identify community-wide respiratory health threats and guide public health interventions.
Environmental Policy: Real-time correlations between environmental conditions and respiratory health provide evidence for air quality regulations and public health advisories.
Healthcare Planning: Predictive analytics inform resource allocation and capacity planning for respiratory care services.
Future Directions and Innovation
Next-Generation Capabilities
Emerging technologies promise even more sophisticated prediction systems:
Multi-Modal Sensor Integration: Combining wearable devices with smart home sensors creates comprehensive health monitoring ecosystems that capture environmental and behavioral factors.
Genetic Integration: Incorporating genetic risk factors into prediction models enables more personalized risk assessment and intervention strategies.
Social Determinants: Including socioeconomic and behavioral data enhances prediction accuracy by accounting for factors beyond pure physiology.
Advanced Analytics
Evolving AI capabilities enable more nuanced health predictions:
Federated Learning: Privacy-preserving machine learning enables model training across multiple institutions without sharing sensitive patient data.
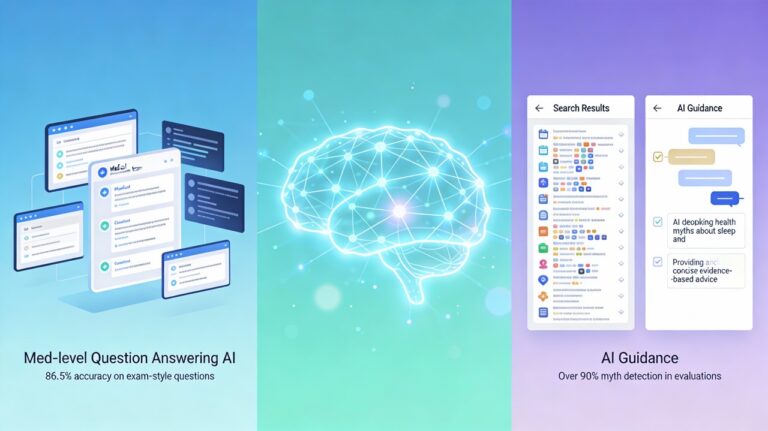
Explainable AI: Interpretable models provide clear explanations for predictions, enhancing clinical trust and enabling better patient education.
Continuous Learning: Models that adapt over time improve accuracy as they accumulate more patient-specific data and outcomes.
Regulatory and Ethical Considerations
FDA Approval and Validation
Clinical deployment requires regulatory oversight:
Medical Device Classification: AI prediction systems may require FDA approval as software-based medical devices, necessitating rigorous clinical validation studies.
Clinical Trial Requirements: Prospective studies demonstrating improved patient outcomes are essential for regulatory approval and clinical adoption.
Post-Market Surveillance: Continuous monitoring of real-world performance ensures prediction systems maintain accuracy and safety standards.
Ethical Implementation
Responsible deployment addresses important ethical considerations:
Health Equity: Ensuring equal access to prediction technology across socioeconomic and demographic groups prevents exacerbation of health disparities.
Informed Consent: Clear communication about prediction limitations helps patients make informed decisions about monitoring and interventions.
Clinical Judgment: Maintaining physician oversight ensures AI predictions supplement rather than replace clinical decision-making.
Wearable Prediction Timeline

Conclusion: A New Era of Predictive Respiratory Care
Smart wearables powered by artificial intelligence represent a transformative breakthrough in chronic respiratory disease management. The ability to predict dangerous exacerbations days before symptoms appear fundamentally changes the therapeutic paradigm from reactive emergency care to proactive prevention.
The compelling clinical evidence—with prediction accuracies exceeding 90% and advance warning windows of 48-72 hours—demonstrates that this technology is ready for widespread clinical deployment. As regulatory frameworks evolve and healthcare systems integrate these tools, millions of patients with asthma and COPD will benefit from earlier interventions that prevent emergency crises.
The implications extend beyond individual patient care to encompass population health management, healthcare cost reduction, and improved quality of life for chronic disease patients worldwide. Smart wearables are not just monitoring devices—they are becoming predictive health partners that can anticipate and prevent medical emergencies before they occur.
The future of chronic disease management is predictive, personalized, and powered by the convergence of wearable technology and artificial intelligence. This transformation promises to save lives, reduce healthcare costs, and restore confidence to millions living with chronic respiratory conditions.